Decoding the Link: How Uric Acid Levels Might Affect Male Testosterone
Okay, so let’s talk about something that’s been a bit of a head-scratcher in the world of men’s health: the connection, or lack thereof, between serum uric acid levels and testosterone levels. You know, that stuff in your blood that can sometimes cause gout, and the hormone that’s pretty key for, well, being a guy.
For a while now, folks have been looking into this, but the results have been, shall we say, all over the map. Some studies said there was a negative link, others a positive one. It was confusing! So, a group of researchers decided to dig into some serious data to see if they could shed some light on the situation.
What’s Uric Acid Anyway?
First off, a quick primer. Serum uric acid (SUA) is basically the end product when your body breaks down purine nucleotides. It might sound like just a waste product, but it actually plays a role. It helps gobble up oxygen free radicals, which is a good thing for keeping your body running smoothly. Think of it as a crucial antioxidant, helping keep things stable, like blood pressure, and fighting off oxidative stress.
But, like many things, too much isn’t great. High SUA levels, or hyperuricemia, are pretty common – affecting over 20% of guys in the US, according to the text. And high SUA has been linked to a bunch of metabolic troubles:
- Obesity
- Type 2 diabetes
- Cardiovascular disease
- Hepatic steatosis (fatty liver)
- Insulin resistance
It seems SUA messes with things like chronic inflammation, oxidative stress, and even how your blood vessels function. Nasty stuff when it’s too high.
And Testosterone?
Now, testosterone. This hormone, made in the testes, is fundamental for male development and characteristics. But low testosterone is becoming a real concern, especially as guys get older. It’s estimated to affect about 7% of men around 50, and more as the years tick by.
Interestingly, low testosterone often shows up alongside those same metabolic issues we just talked about:
- Obesity
- Metabolic syndrome
- Insulin resistance
- Increased risk of Type 2 diabetes
Some studies even suggest that getting testosterone levels back up through therapy can actually help improve things like BMI, insulin resistance, and blood sugar control in men with diabetes and obesity.

The Study’s Mission
Given that both high SUA and low testosterone seem buddy-buddy with metabolic syndrome, it made sense to look closer at their direct relationship. But because past studies were contradictory, these researchers had a hunch that maybe the connection wasn’t just a simple straight line (a linear association). They thought it might be more complicated, perhaps influenced by things like age, metabolic health, and lifestyle.
So, they dove into the data from the National Health and Nutrition Examination Survey (NHANES) from 2011 to 2016. This is a huge survey in the US that collects health and nutrition info. They looked at data from 7791 adult males, aged 18 and older.
What They Found: It’s Not So Simple!
After crunching the numbers and adjusting for a whole bunch of potential confounding factors (like age, race, BMI, liver enzymes, blood pressure issues, diabetes, cholesterol issues, smoking, drinking, and more), they found something pretty interesting.
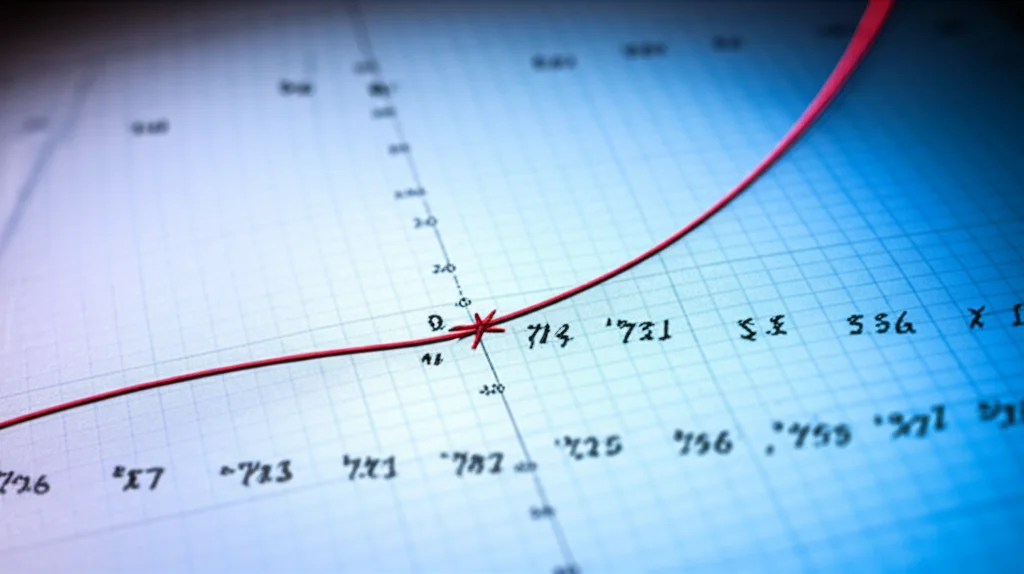
Yes, there was a negative correlation overall – meaning as SUA levels went up, testosterone levels tended to go down. But here’s the kicker: it wasn’t a simple linear relationship across the board. They discovered a non-linear association.
Think of it like a curve, not a straight line. There was an “inflection point” at 4.4 mg/dL for serum uric acid levels.
- Below 4.4 mg/dL: On this side of the point, they didn’t find a statistically significant link between SUA and testosterone. It was kind of… flat.
- Above 4.4 mg/dL: *This* is where the negative correlation kicked in strongly. For guys with SUA levels higher than 4.4 mg/dL, increasing SUA was clearly linked to decreasing testosterone.
So, it seems the negative impact of higher uric acid on testosterone really shows up once your levels cross a certain threshold.
Digging Deeper: Who’s Most Affected?
The researchers also looked at different subgroups of men. They found that the negative link between higher SUA and lower testosterone was particularly strong in certain groups:
- Younger men: The association was more pronounced here. Maybe because younger guys have faster metabolism or more sensitive endocrine systems? The text suggests these possibilities.
- Current alcohol drinkers: The link was stronger in this group.
- Men *without* CKD, diabetes, hypertension, hyperlipidemia, and gout: This is a bit counterintuitive! The negative link was *more* significant in healthier guys compared to those with these conditions. The study doesn’t offer a definitive reason for this, but it’s an interesting finding.
The link was still there for guys with those conditions, but statistically, it was stronger in those who didn’t have them.
Why Might This Be Happening? (Possible Explanations)
Okay, so we see a link, especially above 4.4 mg/dL. But *how* could uric acid influence testosterone? The researchers discussed a few potential mechanisms, though they stressed these aren’t fully understood yet:
- Direct Testicular Damage: Uric acid crystals might deposit in the testes, causing oxidative damage and directly messing with the cells that make testosterone (Leydig cells).
- Metabolic Syndrome Pathway: High SUA can contribute to metabolic syndrome and insulin resistance. These conditions are known to increase the conversion of testosterone into estrogen and reduce testosterone production by the testes. So, SUA could indirectly lower T by fueling metabolic problems.
- Testosterone Influencing SUA: It might even work the other way around! Low testosterone could lead to insulin resistance, which might reduce how well your body clears uric acid, potentially raising SUA levels. Low T might also affect protein breakdown, increasing purine levels and thus uric acid.
It’s likely a complex interplay, not just a one-way street.

Important Caveats
Before we jump to too many conclusions, it’s crucial to remember the limitations of this study, which the researchers were upfront about:
- Cross-Sectional Design: This study looked at data at a single point in time. It shows an *association* (a link), but it absolutely *cannot* prove that high SUA *causes* low testosterone (or vice versa). We need longitudinal studies to figure out cause and effect.
- Generalizability: The data is from the US. The findings might not apply to men of different racial backgrounds or in other parts of the world.
- Single Testosterone Measurement: Testosterone levels fluctuate throughout the day. Measuring it only once might not give a complete picture, and diagnosing low T usually requires multiple measurements.
- Self-Reported Data: Some information (like smoking or drinking habits) was based on what people said, which can sometimes be inaccurate.
- Limited Data: They couldn’t look at free or bioactive testosterone, only total testosterone. They also didn’t specifically study men diagnosed with hypogonadism (very low testosterone).
The Takeaway
So, what’s the bottom line? This study, using a large dataset, suggests that the relationship between serum uric acid and testosterone levels in adult males isn’t a simple linear one. Instead, there seems to be a threshold around 4.4 mg/dL. Below that, no clear link was seen. But above that point, higher uric acid levels were significantly associated with lower testosterone levels. This link was particularly noticeable in younger men, current drinkers, and surprisingly, those without certain existing metabolic conditions.
While the exact mechanisms are still being figured out, this research adds a fascinating piece to the puzzle of men’s metabolic and hormonal health. It highlights that SUA might be another factor to consider when looking at testosterone levels, especially when they are elevated. But remember, this is an association, not proof of cause. More research is definitely needed to fully understand this complex relationship and what it means for overall health.
Source: Springer







