Tiny Bubbles, Big Results: New Tech Boosts Eyedrop Effectiveness
You know, for something as crucial as our eyesight, getting medicine *into* the eye effectively is surprisingly tricky. We’ve all probably used eyedrops at some point, right? You tilt your head back, squeeze, blink a few times, and hope for the best. But here’s a little secret: most of that precious drop doesn’t actually make it where it needs to go. It gets washed away by tears, drained out, or just can’t cross the eye’s natural barriers. We’re talking less than 5% often reaching the target! That means needing frequent drops, which can be annoying, lead to poor compliance, and sometimes cause irritation from all the extra stuff in the drops.
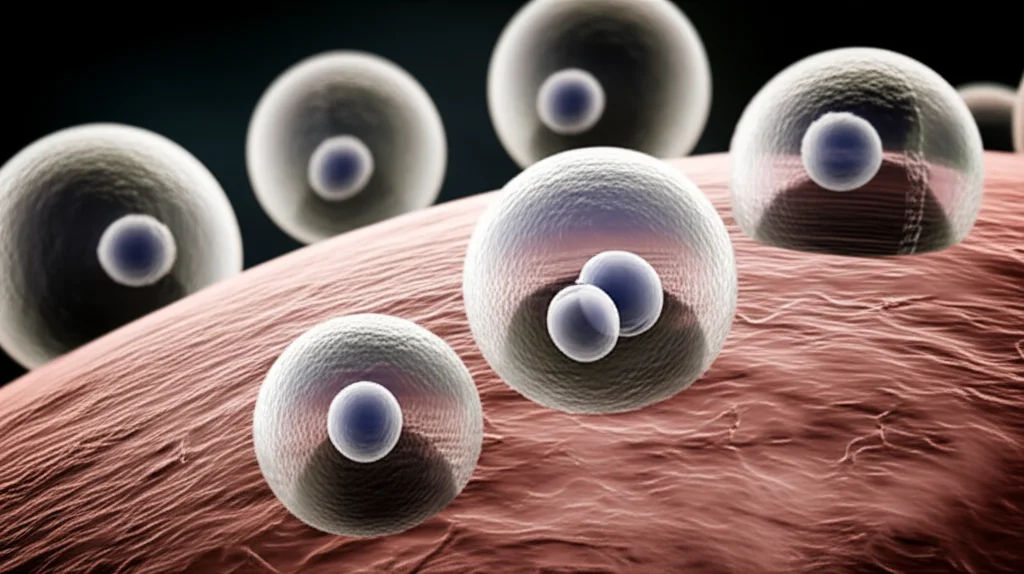
So, the big question is: how do we get more of the good stuff *into* the eye and make it stay there longer? Scientists have been trying all sorts of clever ideas – special contact lenses, gels, tiny particles, you name it. Among these, *liposomes* have been popular. Think of them as tiny fatty bubbles that can carry drugs. They’re pretty good at protecting the drug and helping it hang around, but they’re a bit stiff. They struggle to squeeze through the really tiny gaps in our tissues.
Enter the Transfersomes!
This is where things get interesting. Imagine those liposomes, but make them *super flexible*. That’s essentially what *transfersomes* (TFS) are. They’re like ultra-elastic little bubbles. We add special ingredients called *edge activators* that make their structure really bendy. This flexibility is key because it means they can deform and squeeze through tiny intercellular pores without breaking.
TFS have been a big hit in skin drug delivery – they can wiggle their way through the tough outer layer of skin. They even have this cool ability called “transpore hydrotaxis,” where they can move along water gradients, kind of surfing through the tissue towards wetter areas. Pretty neat, huh?
Eyes vs. Skin: A Different Ballgame
Now, while skin delivery is one thing, eyes are totally different. They’re much more sensitive, and their structure is unique. The skin is tough; the eye surface is delicate. Also, most research on TFS for eyes has only looked at getting drugs through the cornea (the clear front part). But the conjunctiva (the white part and inside the eyelid) and sclera (the outer white layer) are also important routes for drug delivery, and they have different structures and properties. We hypothesized that TFS might behave differently in these different eye tissues.
We were particularly interested in a drug called tonabersat. It’s a hydrophobic (doesn’t like water much) drug that shows real promise for treating eye inflammation, like in dry eye disease. The problem is, its poor water solubility makes it tough to formulate into a standard eyedrop. There’s no eye formulation available commercially yet. We’d already worked on developing tonabersat-loaded TFS eyedrops and showed they were stable and could enhance penetration in a static lab model. But the eye is dynamic – there are tears flowing, tissues changing hydration. So, we needed to see how our TFS would perform in a more realistic setting.
Putting Our Transfersomes to the Test (Ex Vivo, Of Course!)
To figure this out, we decided to use *ex vivo* models. That means using real tissues or organs, but outside of a living body. It’s a great step between basic lab tests and full animal studies.
Here’s what we did:
- Tolerability: We checked if our TFS eyedrops were irritating. We used the HET-CAM test (Hen’s Egg Test on Chorioallantoic Membrane), which is a humane way to check conjunctival irritation using fertilized eggs. We also used the BCOP assay (Bovine Corneal Opacity and Permeability) with cow corneas to see if they caused corneal damage. We compared our TFS and a control formulation (just tonabersat in a medium chain triglyceride, or MCT, solution) to negative controls (like simulated tear fluid) and positive controls (known irritants).
- Wettability: We measured the contact angle of the drops on fresh cow corneas using a goniometer. This tells us how well the drop spreads on the eye surface. A lower contact angle means better spreading and wetting.
- Penetration: This was the big one. We used a whole porcine (pig) eye model. Pig eyes are quite similar to human eyes. We set them up with simulated tear flow and applied our TFS eyedrops and the MCT control. Then, at different time points (0.25, 0.5, 1, and 2 hours), we carefully dissected the eyes into different tissues – cornea, conjunctiva, eyelid, and sclera-choroid – and measured how much tonabersat had gotten into each tissue using a fancy technique called HPLC.

We prepared our TFS using a standard method, ending up with tiny, uniformly sized vesicles. The MCT formulation was just a clear solution.
What We Found: Good News on All Fronts!
First off, the tolerability tests were great. Both our TFS and the MCT control were non-irritating in both the HET-CAM and BCOP assays. They behaved just like the negative control (simulated tears), showing no signs of damage or irritation. This is super important because eye formulations *have* to be gentle.
Next, the contact angle test gave us our first hint that TFS were special. The TFS eyedrop had a lower contact angle than the MCT solution. What does that mean? It means our TFS formulation spread better and wetted the corneal surface more effectively. This is crucial because better wetting means less washout by tears and potentially more time for the drug to penetrate. We think this is partly because the eye surface, covered by the tear film, is hydrophilic (likes water), and our water-based TFS formulation is more compatible with that than the oily MCT. Plus, our TFS had a neutral to slightly positive charge, which helps them interact favorably with the slightly negatively charged corneal surface.
But the really exciting results came from the penetration study in the whole eye model. Despite the simulated tear flow trying to wash things away, our TFS formulation delivered significantly more tonabersat into *all* the ocular tissues we tested compared to the MCT control.
Let’s break it down:
- Cornea: TFS resulted in about 6.6 times higher peak concentration (Cmax) and a whopping 35.5 times higher overall exposure (AUC) over 2 hours compared to MCT. This suggests the flexible TFS are much better at getting through the tight junctions of the corneal epithelium.
- Conjunctiva and Eyelid: This is where the difference was even more dramatic. TFS achieved about 16 times higher Cmax and 17-37 times higher AUC in these tissues. The conjunctiva has a larger surface area and larger intercellular spaces than the cornea, making it more permeable, and the hydrophilic nature of these tissues seems to really help the amphiphilic (partially water-liking, partially fat-liking) TFS penetrate.
- Sclera-Choroid: Again, TFS showed a massive improvement, with Cmax being about 18.6 times higher and AUC an incredible 74.4 times higher than MCT. The sclera is more permeable to hydrophilic things, and our TFS seem to navigate this well, potentially migrating from the conjunctiva into the sclera via that “transpore hydrotaxis” mechanism we mentioned earlier.
Interestingly, even with the simulated tear flow, the peak drug concentration (Tmax) in all tissues seemed to occur *later* with TFS than with MCT. This is great news because it suggests the TFS formulation provides a more sustained release of the drug, potentially reducing the need for frequent dosing.
Our findings really highlight how the composition and flexibility of TFS help them get through the eye’s barriers and target different tissues effectively. We saw how penetration varied across the cornea, conjunctiva, eyelid, and sclera-choroid, confirming our hypothesis that tissue structure matters. The ex vivo model, while not a perfect replica of a living eye (it doesn’t have blinking, systemic clearance, or human-specific anatomy), was incredibly valuable for comparing our formulations head-to-head under controlled, dynamic conditions.

The Takeaway
So, what’s the big picture here? Our study demonstrates that tonabersat-loaded transfersomes are well-tolerated on the ocular surface and are significantly better at getting the drug *into* various eye tissues compared to a simple solution. Their flexibility and interaction with tissue properties allow them to penetrate barriers and potentially provide sustained and targeted delivery.
This opens up a really promising avenue for delivering hydrophobic drugs like tonabersat safely and effectively to the eye, potentially improving treatment outcomes for conditions like dry eye disease and uveitis. Of course, these were ex vivo studies, so the next crucial step is to evaluate these TFS formulations in living animals to confirm these exciting results and check their long-term safety. But for now, we’re pretty thrilled with the potential these tiny, flexible bubbles hold for the future of eyedrop therapy!
Source: Springer







