Cracking the Code on Surgical Leaks: Inside the TENTACLE – Colon Study
Hey There! Let’s Talk About Surgery… And When Things Get Tricky
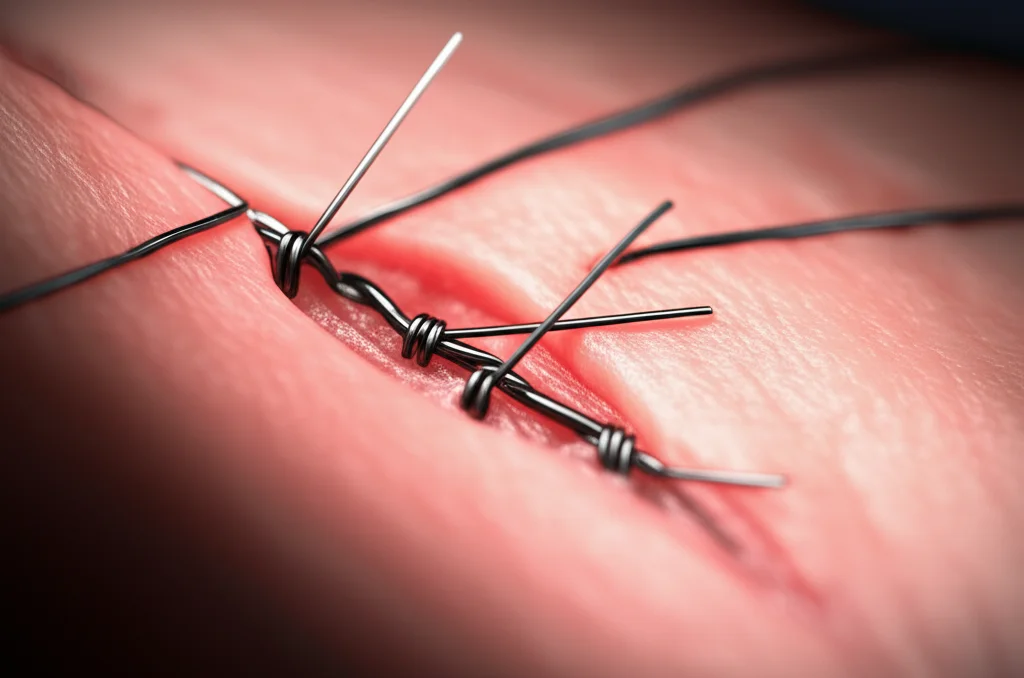
You know, sometimes even the most routine-sounding surgeries can hit a snag. We’re talking about colon cancer resection – a really important procedure for folks dealing with that diagnosis. Doctors remove the part of the colon with cancer and then, ideally, sew or staple the ends back together. This join is called an anastomosis. Most of the time, it heals up just fine, and that’s fantastic news.
But here’s the thing, and it’s a pretty big “but”: sometimes, that join doesn’t heal perfectly. It can leak. And let me tell you, this nasty thing called anastomotic leakage (AL) is a serious complication. We’re not talking about a minor hiccup; this can lead to all sorts of trouble, like needing more surgeries, spending way longer in the hospital (maybe even the ICU), a higher chance of ending up with a permanent stoma (which is a major life change), and sadly, it significantly increases the risk of not making it through.
The Puzzle: Fixing the Leak
What’s wild is, even though AL is a known risk and it’s pretty severe, we don’t have a super clear, one-size-fits-all playbook for fixing it. Right now, how doctors treat a leak often depends on a bunch of things: how sick the patient is, what resources the hospital has, and honestly, what the surgeon prefers or has experience with. The leak itself has different characteristics too – like how big it is, where it is, if there’s infection, etc. But we don’t really know *exactly* how much each of these factors should influence the treatment decision or how they affect the outcome.
Treatment options are varied. They can range from just giving antibiotics and watching closely (conservative management) to draining fluid with radiology, using clips endoscopically, or going back into surgery, sometimes even having to take the join apart and create an ostomy. With so many options and not a lot of solid evidence comparing them, figuring out the *best* way to treat a specific patient with a specific type of leak is a real challenge. It feels a bit like throwing darts in the dark sometimes, and we really need more light!
Enter the TENTACLE – Colon Study!
That’s where this cool, massive project comes in. It’s called the TENTACLE – Colon study, and it’s a huge international effort. Think of it like a global team of doctors and researchers all putting their heads (and their data) together to tackle this problem head-on. They’re running a big retrospective study, which means they’re looking back at the records of patients who had colon cancer surgery and then developed an anastomotic leakage.
Their main goals are super important:
- Goal 1: Build a Crystal Ball (Sort Of!) They want to figure out what factors predict which patients are most likely to have really bad outcomes – specifically, who is at highest risk of dying within 90 days or having severe complications (the kind graded 4 or 5 on the Clavien-Dindo scale, which are pretty serious). They plan to use this information to create and test prediction models. Imagine being able to better identify high-risk patients early on!
- Goal 2: Find the Right Tool for the Job! They want to compare the effectiveness of all those different treatment strategies I mentioned earlier. By looking at a huge number of patients and carefully considering all the different patient, tumour, surgery, and leak characteristics, they hope to see which treatments work best for which types of leaks and patients. This could really help doctors make more personalized, evidence-based decisions.
How They’re Doing It: A Global Data Dive
This isn’t a small undertaking. The TENTACLE – Colon study is aiming to include a whopping 2000 patients who developed AL after colon cancer resection between 2018 and 2022. And it’s truly international, with hundreds of centres from dozens of countries participating. This global reach is a big deal because it means the results are more likely to apply to patients everywhere, not just in one specific hospital or region.
They’re collecting *tons* of detailed information on each patient, including:
- Patient stuff (age, health conditions, smoking, etc.)
- Tumour stuff (type, location, stage)
- Surgery details (how it was done, type of anastomosis, complications during surgery)
- How the leak was diagnosed (timing, symptoms, scans)
- The leak itself (size, location, signs of infection)
- And crucially, *exactly* how the leak was treated (all the different interventions, primary and any subsequent ones).
They’re tracking outcomes like hospital stay, ICU stay, how many times a patient needed another intervention, mortality at different time points (in-hospital, 30-day, 1-year, and that key 90-day mark), overall complication burden, and whether patients are stoma-free after a year.

All this data is being collected using a secure online system, with careful checks to make sure the information is accurate and complete. They’ve even done pilot testing with experts from around the world to refine the process and make sure everyone is on the same page with definitions.
Why This Study is a Big Deal (and a Couple of Caveats)
The biggest strength of the TENTACLE – Colon study is the sheer volume and detail of the data they’re collecting from so many different places. This allows for really robust analysis, letting them look at specific subgroups of patients and leaks to see what works best. It’s designed to fill a major gap in our knowledge because, as we discussed, large comparative studies on AL treatment have been pretty scarce.
Of course, no study is perfect. This one is retrospective, meaning they’re looking back in time. While they’re using sophisticated statistical methods (like regression analysis and propensity score matching) to try and account for differences between patients who received different treatments, there’s always a risk of something called “confounding by indication.” This basically means that patients who got a certain treatment might have been sicker or different in some way that isn’t fully captured by the data, making it hard to say definitively that the treatment *caused* the better or worse outcome. Also, since not *every* hospital in the world is participating, there might be a bit of selection bias, potentially leaning towards data from centres that are more involved in research.

Looking Ahead: What This Means for Patients
Despite the limitations, the potential impact of the TENTACLE – Colon study is huge. The prediction models they develop could give doctors a better tool to assess how severe a patient’s leak is likely to be in terms of mortality risk, right when it’s diagnosed. Currently, severity is often described *after* the fact, based on how it was treated, which isn’t helpful for making decisions in the moment.
Even more exciting are the findings on treatment effectiveness. By identifying which strategies work best for different types of leaks and patients, the study could provide much-needed evidence to guide clinical practice. This could lead to more standardized, yet personalized, treatment plans for patients facing this tough complication, hopefully improving their outcomes and quality of life.
So, while anastomotic leakage after colon cancer surgery remains a challenge, studies like TENTACLE – Colon are vital steps towards understanding it better and finding the best ways to help patients recover. It’s a complex puzzle, but with global collaboration and detailed data, we’re getting closer to cracking the code.
Source: Springer