Stem Cells Fight Back: Restoring Ovarian Health After Chemo
Hey there! Let me tell you about something pretty exciting happening in the world of medicine, specifically for women facing a tough challenge called Premature Ovarian Insufficiency, or POI.
What’s the Big Deal with POI?
Imagine this: POI is when a woman’s ovaries decide to retire way too early, usually before she even hits 40. This isn’t just about fertility, although that’s a huge part of it. It messes with your hormones, which can lead to all sorts of long-term issues like weaker bones, heart problems, and even affect your mood. Right now, we don’t really have a magic bullet to fix the damaged ovaries themselves. Current treatments mostly focus on managing the symptoms, not bringing the function back. And for folks who go through chemotherapy, this is a really common and heartbreaking side effect.
Enter Stem Cells: Our Little Helpers
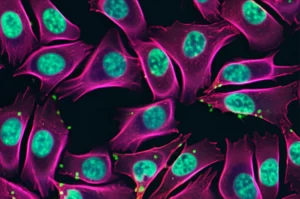
You’ve probably heard of stem cells, right? They’re like these amazing blank slates in our bodies that can turn into different cell types and help repair things. Mesenchymal Stem Cells, or MSCs, are a type of adult stem cell that are particularly good at regenerating tissue and calming down inflammation. They’ve shown *loads* of promise in regenerative medicine.
Umbilical cord MSCs (UC-MSCs) have been a popular choice because they’re relatively easy to get and they grow pretty well. We’ve seen studies where UC-MSCs seem to boost hormone levels, reduce follicle loss, stop ovarian cells from dying off (apoptosis), and prevent scarring. That sounds great, and there are tons of clinical trials looking into them!
But Here’s the Catch…
While UC-MSCs are cool, they’re not perfect. Think about it – they come from different donors, so there’s a lot of variability. Plus, they don’t multiply forever, and their ability to differentiate or function can drop off after they’ve been grown in the lab for a while. This inconsistency can make it tricky to get reliable results, especially when we’re thinking about using them widely. We really need a source of MSCs that’s more consistent, can be produced in large amounts, and stays potent.
The Power of Pluripotency and a Sneaky Intermediate
This is where Human Pluripotent Stem Cells (hPSCs) come into the picture. These are the real blank slates, like Human Embryonic Stem Cells (hESCs) or Human Induced Pluripotent Stem Cells (hiPSCs). They can basically become *any* cell in the body and they can grow *indefinitely* in the lab. This makes them a dream source for making tons of high-quality MSCs.
The trick is making sure they differentiate safely into the right kind of cells without any rogue pluripotent cells hanging around (because those can cause tumors). Scientists have been working on protocols to guide hPSCs specifically towards MSCs. Traditionally, this often involved going through a “mesoderm” stage.
But what if there’s another route? Enter the *Neural Crest Cells* (NCCs). These are fascinating cells that pop up very early in development and are multipotent, meaning they can turn into several different cell types, including MSCs. What’s *really* interesting is that NCCs have been found near developing ovaries and seem to play a role in how the ovaries get their nerve supply, which is important for follicle formation and function. This got us thinking: maybe MSCs derived from hPSCs *via* this neural crest pathway (hPSC-NCC-MSCs) could be particularly good for ovarian repair!
Our New Recipe for Super Stem Cells
So, we decided to cook up a new, faster way to get MSCs from hPSCs using NCCs as the stepping stone. We tweaked an existing protocol that uses some special small molecules, CHIR99021 and SB431542, which help push the hPSCs towards becoming NCCs efficiently.
We used a couple of different hESC lines (H1 and H9) and also some hiPSCs. We found that our modified method, especially using 1 µM CHIR99021 and 0.5 µM SB431542, was really effective at turning hPSCs into NCCs within just 7 days. We checked this by looking at their shape and seeing that they started expressing the right NCC markers like P75, HNK1, SOX10, and AP2α, while losing their original pluripotency markers. The H1-hESC line was particularly good at this, giving us the highest efficiency of NCCs.

Once we had these NCCs, we then nudged them further to become MSCs using a different culture medium. Within about 20 days, they started looking like the typical fibroblast-like MSCs we recognize.
Meet Our New MSCs: The H1-NCC-MSCs
We put these new hPSC-NCC-MSCs through their paces to see if they were the real deal. And guess what? They checked all the boxes!
- They had the right MSC surface markers (like CD29, CD44, CD73, CD90, CD105) and *didn’t* have the blood cell markers (CD34, CD45), just like they should.
- They could differentiate into bone cells (osteoblasts), fat cells (adipocytes), and cartilage cells (chondrocytes) in the lab, proving they are multipotent. Interestingly, they seemed even better at becoming bone cells compared to UC-MSCs.
- And here’s the really exciting part: the H1-NCC-MSCs showed *superior* growth rates and *much better* resistance to aging in the lab compared to both hiPSC-derived MSCs and UC-MSCs. Even after 15 passages (that’s a lot of multiplying!), the H1-NCC-MSCs kept their youthful appearance and high proliferation rate, while the UC-MSCs started looking tired and showing signs of senescence.
This enhanced proliferative capacity and anti-aging potential make H1-NCC-MSCs a really promising candidate for therapy, especially since you need a good number of cells for treatment.
Putting Them to the Test in Real Life (Well, in Rats)
Okay, lab tests are great, but the real question is: do they actually *work* to fix POI? To find out, we used a rat model where we induced POI using chemotherapy (cyclophosphamide, or CTX), which mimics what happens to human patients. We then transplanted either H1-NCC-MSCs or UC-MSCs into these rats and compared them to a control group and a POI group that didn’t get stem cells.
The results were pretty encouraging!
- Rats treated with either type of MSC started recovering their body weight and, importantly, their normal estrous cycles (a sign of ovarian function) compared to the untreated POI group.
- Their ovaries, which had shrunk after chemo, started to regain size and weight.
- Looking inside the ovaries, the number of follicles (those little structures that contain eggs) was significantly reduced in the POI group, but MSC treatment helped restore the count, including the crucial primordial follicles.
- Hormone levels also improved. E2 (estradiol) and AMH (anti-Müllerian hormone), which drop in POI, went up after MSC treatment, while FSH (follicle-stimulating hormone), which goes up in POI, went down.
- And the ultimate test: fertility! The rats treated with MSCs had significantly larger litter sizes compared to the untreated POI group.
Both H1-NCC-MSCs and UC-MSCs showed comparable effectiveness in restoring ovarian function and fertility in this rat model. This is a big deal – it means our new hPSC-NCC-MSCs are *at least* as good as the current go-to UC-MSCs in a living system, with the added benefit of being more consistent and renewable. We also checked for any signs of toxicity, and thankfully, the H1-NCC-MSCs seemed safe in the rats.

How Do They Work Their Magic?
We also wanted to understand *how* these stem cells were helping. We noticed that the transplanted MSCs tended to hang out *around* the ovarian follicles, rather than turning *into* follicular cells themselves. This strongly suggests they’re working through a “paracrine” effect – basically, they’re secreting helpful factors that signal to the nearby ovarian cells.
To test this, we collected the liquid medium that the MSCs had been growing in (called conditioned medium, or CM), which contains all these secreted factors. We then added this CM to ovarian granulosa cells (GCs) in the lab that we had damaged with a chemo drug (4-HC, a cyclophosphamide metabolite).
The results were clear:
- GCs treated with the chemo drug alone looked sick and irregular. But when we added CM from either H1-NCC-MSCs or UC-MSCs, the GCs started looking much healthier.
- The chemo drug caused a lot of GC death (apoptosis), but the MSC-CM significantly reduced this cell death.
- The MSC-CM also boosted the viability (health and survival) of the damaged GCs.
- We saw changes in key proteins related to apoptosis, confirming that the CM was actively preventing cell death.
This confirmed that the MSCs are likely helping by sending out protective signals to the ovarian cells.
Fighting Off Stress and Boosting Energy
Chemotherapy often damages cells by causing a lot of oxidative stress – basically, creating harmful molecules called Reactive Oxygen Species (ROS) and overwhelming the cell’s natural defenses. This can really mess up the mitochondria, the cell’s powerhouses.
We hypothesized that the MSCs were also helping by reducing this stress. And our experiments in the lab with the damaged GCs confirmed it!
- The chemo drug caused a big spike in ROS levels, but the MSC-CM treatments significantly brought those levels down.
- Mitochondria in the damaged GCs were struggling, losing their membrane potential (a sign they’re not working right). MSC-CM helped restore this potential, suggesting improved mitochondrial health.
- We also measured levels of oxidative damage (MDA) and antioxidants (GSH and SOD). The chemo drug increased damage and decreased antioxidants, but MSC-CM reversed these trends, boosting the cell’s ability to fight stress.
So, it seems a big part of the MSCs’ protective effect is by acting as powerful antioxidants and helping the ovarian cells’ mitochondria recover. Again, both H1-NCC-MSC-CM and UC-MSC-CM showed similar benefits, although H1-NCC-MSC-CM seemed slightly better at reducing apoptosis and oxidative stress in the lab, though not statistically significantly in all measures.

Looking Ahead: The Future is Bright (But Needs More Work!)
This study gives us some really exciting news. We’ve developed a faster, more efficient way to create MSCs from hPSCs using the neural crest route. These hPSC-NCC-MSCs, particularly those from the H1 hESC line, are not only easy to produce in large numbers but also have amazing growth and anti-aging properties compared to UC-MSCs.
Crucially, we’ve shown for the first time that these hPSC-NCC-MSCs have therapeutic potential comparable to UC-MSCs in treating chemotherapy-induced POI in rats. They do this by protecting the vital granulosa cells in the ovaries, reducing cell death, alleviating oxidative stress, and improving mitochondrial function, likely through those helpful factors they secrete.
Now, we’re not saying this is the absolute final answer yet. There are still things to figure out. For instance, the culture medium we used still contains animal products (FBS), and for clinical use, we’d need a “xeno-free” version. We also need to dive deeper into *exactly* which secreted factors are doing the heavy lifting and compare these NCC-derived MSCs to hPSC-MSCs made through other pathways. And while the results in rats are promising, translating this to humans always requires more research.
But honestly? The fact that we can create a potentially inexhaustible and stable source of MSCs that works just as well (or maybe even a little better *in vitro*) than current options for a condition with no real cure is incredibly hopeful. This study provides strong evidence supporting the potential of hPSC-NCC-MSCs as a novel therapy for POI. It feels like we’re one step closer to giving women who’ve faced the challenge of chemotherapy a better chance at restoring their ovarian health.
Source: Springer