Tooth Power! How Dental Pulp Stem Cells Could Be a Game Changer for Pollution-Induced Asthma
Alright folks, let’s chat about something that affects millions around the globe: asthma. It’s that frustrating chronic inflammatory disease that makes breathing a real challenge, often involving pesky things like excessive mucus and airways that just won’t behave. And guess what makes it even worse? Our old friend, air pollution, specifically that fine particulate matter, PM2.5. These tiny particles are small enough to sneak deep into our lungs and really stir up trouble.
The PM2.5 Problem and the Search for Solutions
We know PM2.5 exposure seriously ramps up respiratory issues, especially for those already dealing with asthma. This highlights a pretty urgent need for new ways to help people breathe easier when the air quality is poor. Traditional treatments are there, but finding something that tackles the *root cause* of the inflammation triggered by pollution? That’s the golden ticket.
Introducing Our Potential Heroes: Dental Pulp Stem Cells
So, what if I told you that something found right inside your teeth could hold a key? We’re talking about human dental pulp stem cells, or hDPSCs. These are a type of mesenchymal stem cell (MSC), and MSCs are pretty cool because they’re like versatile repair kits for the body. They’ve shown promise in lots of different areas because of their ability to calm inflammation and modulate the immune system. DPSCs, specifically, are easy to get (think wisdom teeth or baby teeth!), don’t have the same ethical debates as some other stem cells, and are generally well-tolerated by the body. They’re known for being potent anti-inflammatories.
Unpacking the Science: What Did We Do?
In this study, we really wanted to see if these amazing hDPSCs could help mice with asthma that was made worse by PM2.5 exposure. We used a standard mouse model where we induced asthma using ovalbumin (a common allergen) and then added in the PM2.5 challenge to mimic that pollution-induced exacerbation. We then gave some of these mice hDPSCs intravenously. We also had a group that received MCC950, which is a known inhibitor of a specific inflammatory pathway called NLRP3 – think of it as our positive control to see if hDPSCs were working on a similar mechanism.
We looked at a bunch of things: how well the mice could breathe (pulmonary function), what their lung tissue looked like under a microscope (histopathology), what kind of cells and inflammatory markers were in their lung fluid (cytology and molecular analysis). We were particularly interested in a process called pyroptosis.
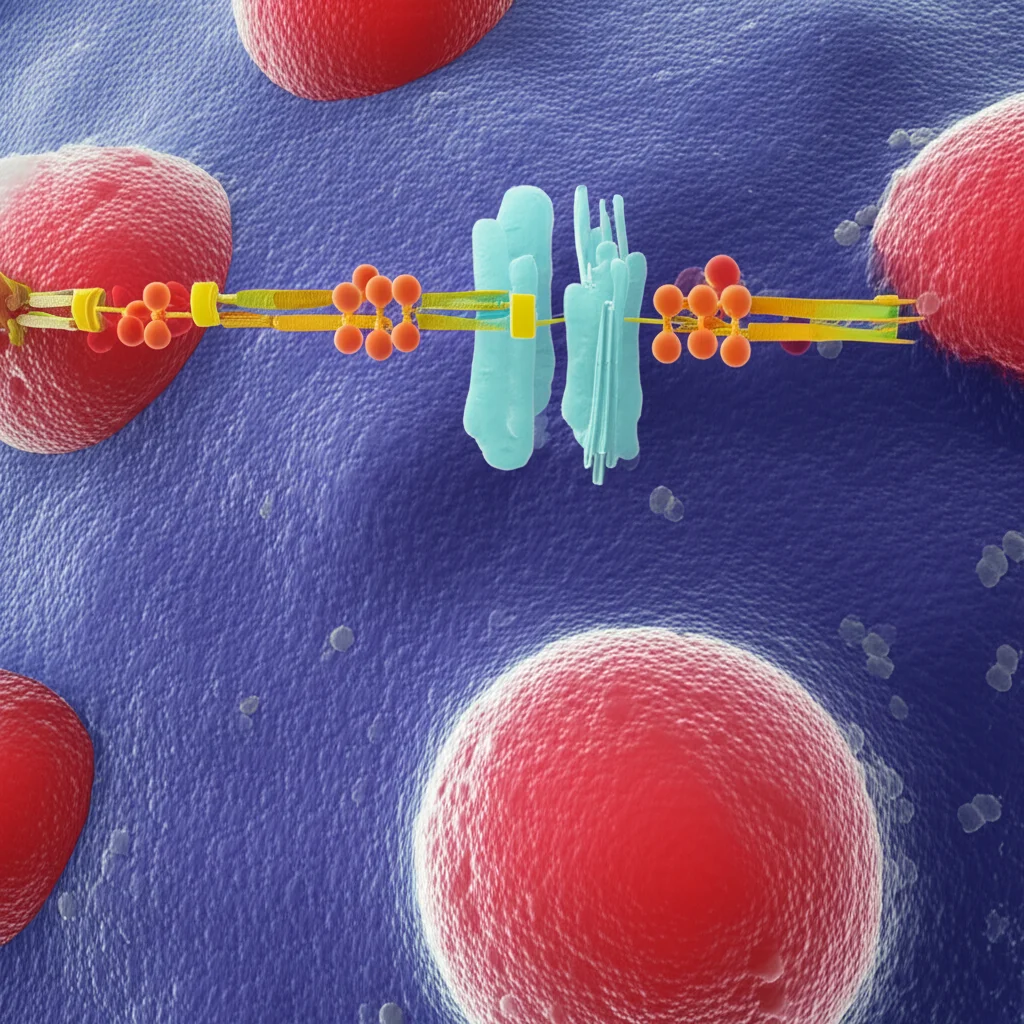
Pyroptosis: The Fiery Cell Death
Okay, let’s get a little sciency for a second. Pyroptosis is a specific type of cell death that’s super inflammatory. It’s like the cell explodes and spills inflammatory signals everywhere, really fanning the flames of inflammation. A key player in this process is something called the NLRP3 inflammasome. When PM2.5 gets into the lungs, it can activate this NLRP3 inflammasome. This activation sets off a chain reaction involving proteins like caspase-1 and GSDMD, ultimately leading to the cell bursting and releasing inflammatory molecules like IL-1β and IL-18. This whole pyroptosis pathway is strongly linked to respiratory diseases, including asthma exacerbations caused by PM2.5. So, targeting this pathway seemed like a smart move.
The Exciting Results: hDPSCs to the Rescue!
So, what did we find when we gave the mice hDPSCs? The results were pretty encouraging!
- Less Inflammation: The hDPSCs significantly reduced the overall airway inflammation in the mice lungs. When we looked at the tissue, there were fewer inflammatory cells hanging around the airways and blood vessels compared to the mice that only got PM2.5 and OVA.
- Improved Lung Function: The mice treated with hDPSCs showed better airway responsiveness, meaning their airways weren’t as hyperreactive when challenged, which is a big deal in asthma.
- Calming the Immune Storm: Allergic asthma involves a specific type of immune response called the Th2 response. PM2.5 made this worse, increasing markers like IL-5 and IL-13, and raising IgE levels (those allergy antibodies) in the blood. hDPSCs dramatically lowered these markers and also reduced the number of eosinophils (a type of inflammatory cell common in asthma) in the lung fluid. Interestingly, the MCC950 control didn’t have as broad an effect on these Th2 markers, suggesting hDPSCs might be doing even more than just hitting the NLRP3 pathway.
- Reduced Mucus: Excessive mucus is a hallmark of asthma. The hDPSCs helped reduce the proliferation of mucus-producing cells and the amount of mucus secretion in the airways.
- Protecting the Barrier: PM2.5 can damage the lung’s epithelial barrier, leading to protein leakage into the airways. hDPSCs helped protect this barrier, reducing the amount of protein found in the lung fluid.
How Did They Do It? Taming the Pyroptosis Fire
Now for the *how*. We dug into the pyroptosis pathway. In the mice exposed to PM2.5, we saw increased levels of the key players in the NLRP3/caspase-1/GSDMD pathway – NLRP3 itself, caspase-1, GSDMD, and the cleaved (active) form of caspase-1, as well as the inflammatory outputs IL-1β and IL-18.

When we administered hDPSCs, they significantly *reduced* the expression of these pyroptosis-related proteins. Their effect on these specific markers was actually quite similar to what we saw with MCC950, the NLRP3 inhibitor. This strongly suggests that one of the main ways hDPSCs are working their magic is by putting a stop to this inflammatory pyroptosis process triggered by PM2.5. They seem to be stepping in and telling the NLRP3 inflammasome to calm down, preventing the whole cascade of cell death and inflammation.
Why This is Exciting
This is pretty big news! It’s the first time we’ve seen evidence that hDPSCs can help with asthma exacerbation caused by PM2.5 inhalation, and it points to a specific mechanism – inhibiting the pyroptosis pathway. Given how widespread asthma is and how much air pollution impacts it, finding a potential cell-based therapy like this is incredibly promising.

Think about it – stem cells from your teeth potentially helping you breathe better when pollution hits hard. It’s a novel approach that tackles the inflammation in a way that current treatments might not fully address, especially the specific inflammatory cell death pathway activated by PM2.5.
Looking Ahead
Of course, science is a journey. This was a study in mice, and there are always steps needed to see if these findings translate to humans. We also noted a couple of limitations, like not having a group that just got hDPSCs without the OVA/PM2.5 model to compare against (though the control groups give us a good baseline), and needing more detailed studies to figure out the exact cellular signals between the hDPSCs and the lung cells. But overall, the picture is clear: hDPSCs show significant potential as a novel therapy for pollution-aggravated asthma by calming down that fiery pyroptosis pathway. It’s definitely something to keep an eye on!
Source: Springer







