The Silent Guardian: How a Lost Protein Fuels Oral Cancer Spread
Hey Everyone, Let’s Talk About Oral Cancer
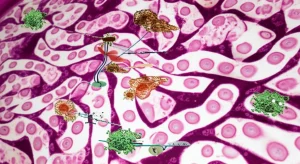
So, you know how our bodies are just incredibly complex machines, right? Everything has a job, from the biggest organs down to the tiniest proteins. And sometimes, when one of those tiny players goes missing or gets silenced, things can go seriously wrong. Today, I want to dive into a fascinating piece of research about oral squamous cell carcinoma (OSCC), the most common type of oral cancer. It’s a tough one, often aggressive and prone to spreading, especially to the lymph nodes, and honestly, the survival rates aren’t where we want them to be, despite all the treatments we have.
That’s why folks in the science world are constantly looking for new clues, new targets, new ways to understand and fight this disease. And this study I’ve been reading about? It shines a spotlight on a protein called SCEL. Now, SCEL isn’t just any protein; it’s usually a key player in building strong epithelial barriers, like the lining of your mouth. Think of it as part of the structural support team, important for things like cell differentiation and keeping cells stuck together properly. But what happens when this team member is missing in action?
SCEL Goes Missing in Action
The first big finding from this research is pretty striking: SCEL is significantly *downregulated* in OSCC. That means there’s a lot less of it in cancer tissues and cells compared to healthy oral tissue. Using fancy techniques like qRT-PCR and IHC (that’s basically looking at gene and protein levels), the researchers confirmed this drop. And it’s not just a random occurrence; they found that lower levels of SCEL correlated with less differentiated tumors (which are generally more aggressive) and, importantly, with lymph node metastasis. It’s like when the structural support goes weak, the building starts to crumble and spread its pieces around.
They even looked at how SCEL levels changed as the cancer progressed, from normal tissue to pre-cancerous lesions and then full-blown cancer, and saw a clear trend: SCEL levels kept dropping. This strongly suggests that losing SCEL isn’t just a side effect of cancer; it might actually be *driving* the progression.

Putting SCEL Back: The “Good Guy” Effects
Okay, so if SCEL is low in cancer, what happens if you boost its levels? The researchers did some cool experiments in the lab, adding SCEL back into OSCC cells. And guess what? SCEL acted like a total tumor suppressor! Here’s what they saw:
- Slower Growth: Cells with more SCEL didn’t proliferate as much. Both in petri dishes and in mouse models, tumors grew slower and were smaller when SCEL was boosted.
- More Cell Death: SCEL significantly increased apoptosis, which is basically programmed cell suicide. It’s like telling the rogue cancer cells, “Alright, your time is up.”
- Cell Cycle Arrest: SCEL seemed to mess with the cell cycle, specifically causing cells to get stuck in the S and G2/M phases. This is like hitting the brakes on their rapid division.
- Increased ROS: They also found that SCEL increased levels of Reactive Oxygen Species (ROS). While ROS can be damaging, in cancer cells, increased ROS can trigger cell death pathways, contributing to the anti-tumor effect.
These findings strongly suggest that SCEL is a crucial brake pedal on OSCC cell growth and survival.
Stopping the Great Escape: Migration and Invasion
Cancer isn’t just a local problem; its ability to migrate and invade other tissues is what makes it so dangerous. This often involves a process called Epithelial-Mesenchymal Transition (EMT), where epithelial cells lose their ‘sticky’ properties and become more like mobile, invasive mesenchymal cells. Think of it as cells changing their identity to become better travelers.
The study found that SCEL is a major roadblock for this escape act. When SCEL levels were high, OSCC cells were much less able to migrate (move across a surface) and invade (push through a barrier like Matrigel, mimicking tissue). How does it do this? SCEL seems to *reverse* the EMT process, promoting MET (Mesenchymal-Epithelial Transition), making cells ‘sticky’ and less mobile again.
And here’s where a big molecular pathway comes in: the TGF-β/Smad pathway. This pathway is a known driver of EMT and cancer progression. The researchers discovered that SCEL overexpression significantly *inhibited* the activity of this pathway. So, it seems SCEL puts the brakes on migration and invasion largely by shutting down this pro-EMT signaling highway.

The Link to Metastasis and Chemotherapy
Since SCEL inhibits migration and invasion, it makes sense that it might also affect metastasis, especially to lymph nodes. The study looked at VEGFC, a marker often associated with lymph node metastasis. They found that VEGFC levels were high where SCEL levels were low, particularly in metastatic tissues. They also showed that the TGF-β/Smad pathway can induce VEGFC expression. This suggests that when SCEL is lost, the TGF-β/Smad pathway gets activated, potentially leading to increased VEGFC and promoting lymph node spread. It’s a chain reaction of bad events triggered by SCEL’s absence.
But there’s a silver lining! The study also explored how SCEL affects sensitivity to chemotherapy, specifically cisplatin (CDDP), a common drug for OSCC. Turns out, increasing SCEL levels made the OSCC cells much *more* sensitive to CDDP. This is huge! It suggests that restoring SCEL might not only slow the cancer down but also make our existing treatments more effective.
The Tiny Culprit: Enter miR-5696
So, we know SCEL is a good guy that’s missing in action. But *why* is it missing? Science often points to tiny regulators called microRNAs (miRNAs). These little molecules can silence genes by binding to their mRNA. Using prediction tools, the researchers identified miR-5696 as a potential culprit targeting SCEL.
And the evidence is compelling! miR-5696 is *highly expressed* in OSCC tissues and cells, showing a clear inverse relationship with SCEL levels (when one is high, the other is low). Lab experiments confirmed that miR-5696 can directly bind to and silence SCEL expression. Furthermore, mimicking miR-5696 in cells boosted proliferation and invasion, while blocking miR-5696 had the opposite effect, just like boosting SCEL did. This points to miR-5696 as a key reason why SCEL is silenced in OSCC, allowing the cancer to progress unchecked.

What Does This All Mean?
Putting it all together, this study paints a pretty clear picture: SCEL acts as a vital tumor suppressor in OSCC. When it’s lost (potentially silenced by miR-5696), it removes a critical brake on cell growth, survival, and most importantly, the ability of cancer cells to become invasive and spread, largely by unleashing the TGF-β/Smad pathway.
The implications are exciting. Finding low SCEL levels could potentially be used for early diagnosis or predicting how aggressive a tumor might be. And, perhaps more thrillingly, the findings suggest new therapeutic avenues. Imagine developing treatments that:
- Boost SCEL expression in tumor cells.
- Block the activity of miR-5696.
- Target the TGF-β/Smad pathway, potentially in combination with strategies to restore SCEL.
These approaches could help restore the body’s natural defenses against OSCC progression and potentially make existing chemotherapy more effective. Of course, there’s always more to learn – the researchers note that other things like DNA methylation could also be silencing SCEL – but this study provides a really solid foundation for understanding SCEL’s critical role and exploring these promising new therapeutic strategies.
It’s a reminder that even the seemingly small players in our cellular world can have massive impacts on our health. Understanding them is the first step to finding new ways to fight tough diseases like OSCC.
Source: Springer