Cracking the Code of a Tough Foe: A Single-Cell Journey into Esophageal Small Cell Carcinoma
Hey there! Let me tell you about something pretty fascinating happening in the world of cancer research, specifically concerning a really tricky type called Small Cell Carcinoma of the Esophagus, or SCCE for short. Now, SCCE isn’t as common as some other esophageal cancers, but boy, is it aggressive. It’s like that stealthy, fast-moving villain in a movie – often caught late, and sadly, it doesn’t give folks a lot of time. We’re talking a median survival of just 8-13 months for many patients. Pretty grim, right?
For years, we’ve been trying to understand this tough cookie better. We’ve looked at its genetics, compared it to other cancers, and even peeked at its immune environment using older methods. But honestly? There’s been a big piece of the puzzle missing. We needed a way to see the *whole* picture, cell by cell, to really get a handle on what makes SCCE tick and, more importantly, how we might fight it better.
That’s where this incredible study comes in. Imagine taking a complex ecosystem – like a bustling city or a dense forest – and trying to understand it by looking at it from a distance. You get some idea, but you miss all the intricate interactions between individual inhabitants. Single-cell transcriptomics is like suddenly being able to zoom in and see *every single cell*, understand what it’s doing, who it’s talking to, and how it fits into the bigger picture. This study did just that for SCCE, and it’s the first time anyone has done it on this scale, looking at samples from 10 SCCE patients, plus others with a more common type (ESCC) and normal tissue for comparison. It’s like getting a high-definition map of this previously mysterious territory.
Diving into the Tumor Microenvironment (TME)
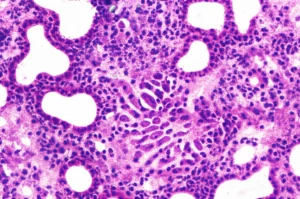
So, what did this super-detailed map show us? Well, first off, it gave us a really clear look at the Tumor Microenvironment (TME) in SCCE. Think of the TME as the tumor’s neighborhood – it’s not just cancer cells, but also immune cells, blood vessels, connective tissue cells, and all sorts of other players hanging around. And this neighborhood can totally influence how the tumor grows and how it responds to treatment.
What we saw was pretty striking when comparing SCCE’s neighborhood to that of ESCC (the more common esophageal cancer). SCCE seems to have a more *immune suppressive* vibe going on. We found a lot of activated regulatory T cells (Tregs), which are basically the immune system’s peacekeepers, telling other immune cells to calm down. While ESCC had more of those ‘exhausted’ CD8+ T cells – the ones that *want* to fight the cancer but are worn out – SCCE had fewer of these but more of the cells putting the brakes on the fight. This suggests that just revving up the immune system might be tougher in SCCE than in ESCC.
But that wasn’t the whole story. We also noticed something else prominent in the SCCE TME: a strong *vessel-induced niche*. This points towards a significant role for angiogenesis – the formation of new blood vessels – in SCCE. ESCC, on the other hand, seemed to lean more towards lymphangiogenesis (new lymph vessels). This difference in the TME landscape is a big deal because it hints at different vulnerabilities for these two types of esophageal cancer.

The Angiogenesis Story in SCCE
Let’s zoom in on that vessel-induced niche in SCCE, because it’s a really exciting finding. This study identified a specific crew of cells that seem to be working together to build and support new blood vessels within the SCCE tumors. We’re talking about:
- FCN1+ macrophages: These are types of immune cells (macrophages) that are hanging out in the tumor and expressing a specific marker (FCN1). They seem to be involved in promoting vessel growth.
- ESM1+ endothelial cells: These are the cells that make up the blood vessel walls, and they’re showing high levels of ESM1, a protein known to be important for angiogenesis and vascular permeability. They look like the “tip-like” cells that lead new vessel sprouts.
- RGS5+ pericytes: These cells wrap around blood vessels and help stabilize them. The ones in SCCE are expressing RGS5 and seem to be closely linked to those ESM1+ endothelial cells.
What’s cool (and concerning, from a cancer perspective) is the strong communication happening between these cells, particularly between the FCN1+ macrophages and the ESM1+ endothelial cells. They’re talking via signals like VEGF-VEGFR interaction, which is a classic pathway for driving angiogenesis. Think of it as them having a private chat channel dedicated to building more roads (blood vessels) for the tumor to get supplies and spread.
This finding is a big “Aha!” moment. Because if angiogenesis is so key to SCCE’s survival and growth, maybe targeting those new blood vessels could be an effective treatment strategy. The study even mentions a real-life case where a patient with advanced SCCE who wasn’t responding well to other treatments saw their disease controlled after adding an anti-angiogenesis drug called Anlotinib. Now, that’s just one case, but it provides compelling early evidence that this might be a promising path forward.
Unpacking TME Ecotypes
Beyond just looking at individual cell types, the study also grouped the non-cancer cells in the TME into what they called “ecotypes.” Think of these as different “communities” or “neighborhood types” within the overall tumor environment, each with its own unique mix of cells and activities. They identified five of these ecotypes (EC1 through EC5).
One ecotype, EC1, really stood out because it was highly enriched specifically in SCCE samples. This EC1 community was characterized by a lot of neutrophils (another type of immune cell, often associated with inflammation) and certain T cell clusters, including resident and exhausted T cells. When they looked at what genes were active in this ecotype, it pointed strongly towards neutrophil activation and cellular chemotaxis (cells moving around).
Interestingly, in an independent group of SCCE patients, having a strong EC1 signature was associated with *better* clinical benefit and overall survival, particularly in one molecular subtype of SCCE (SCCE-A). This is a bit counter-intuitive because neutrophils are sometimes thought to help tumors, but it highlights the complex and sometimes contradictory roles these cells can play. It suggests that maybe, in the context of SCCE, certain types of activated neutrophils within the EC1 ecotype might actually be trying to fight the tumor. These ecotypes give us a brand new way to classify the TME and potentially find biomarkers that predict how a patient might respond to different treatments.

Heterogeneity within the Cancer Cells
Okay, so we’ve talked about the neighborhood around the tumor. Now, let’s talk about the tumor cells themselves – the epithelial cells. Even within SCCE, these cancer cells aren’t all the same. They have their own internal diversity, or “heterogeneity.”
SCCE is known as a “neuroendocrine” carcinoma, meaning its cells have some features similar to nerve or hormone-producing cells. The study confirmed this, finding that SCCE epithelial cells highly expressed classic neuroendocrine markers like NEUROD1 and ASCL1, while ESCC cells expressed markers related to squamous cells (skin-like cells).
They also looked at how these cancer cells interact with their neighborhood. SCCE cells seemed to be chatting more with immune and myeloid cells, while ESCC cells talked more to stromal (connective tissue) and immune cells. Different conversation partners, leading to different neighborhood dynamics!
To really dig into the heterogeneity *within* SCCE cells, the researchers went beyond just looking at those classic markers. They identified eight different “transcriptional metaprograms” (MPs). Think of these as recurring patterns of gene activity within the cancer cells, each representing a fundamental biological process the cells are engaged in.
One of these, MP5, was strongly linked to the neuroendocrine phenotype and, unfortunately, to *poor* clinical survival. Other MPs were related to cell cycle, stress responses, inflammation, and even pathways like KRAS signaling. What was really interesting was finding that MP5 (the neuroendocrine one) seemed to be mutually exclusive with MPs related to inflammation and apoptosis (cell death). This suggests that the more strongly neuroendocrine the cancer cells are, the less likely they are to be involved in inflammatory responses or programmed cell death, which sounds like a recipe for aggressive growth. They even found a cluster of SCCE cells that didn’t express *any* of the classic neuroendocrine markers, present in nearly all patients – adding another layer of complexity!
What Does This All Mean for Treatment?
So, pulling it all together, what does this incredibly detailed single-cell map tell us about how to treat SCCE?
First, the strong evidence of an *angiogenesis-induced niche* is a major takeaway. The crosstalk between macrophages, endothelial cells, and pericytes creating this pro-vessel environment suggests that anti-angiogenesis therapies, like the one used in the case study (Anlotinib), could be a very promising avenue. Given the biological similarities between SCCE and Small Cell Lung Cancer (SCLC), where anti-angiogenesis drugs have shown some benefit, this makes a lot of sense and is definitely something worth exploring further in clinical trials for SCCE.
Second, while SCCE seems more immune suppressive than ESCC overall, the picture for immunotherapy isn’t completely bleak. The study noted that SCCE still had some of those potentially immune-reactive CXCL13+ T cells, and previous work by this team found that a decent percentage of SCCE patients have PD-L1 expression, which is a marker often associated with response to immunotherapy. So, while maybe not as universally applicable as for ESCC, immunotherapy might still benefit a subset of SCCE patients. More clinical data is definitely needed here!
Finally, understanding the *heterogeneity* within the cancer cells themselves (the MPs) and the different TME *ecotypes* gives us potential new biomarkers. Identifying patients whose tumors have a strong MP5 signature (linked to poor survival) or a dominant EC1 ecotype (linked to better survival in one cohort) could help doctors tailor treatments in the future. It reminds us that not all SCCE tumors are the same, and a one-size-fits-all approach might not be the best.

A Look Ahead
Now, it’s important to be realistic. This was a groundbreaking study, the first of its kind for SCCE, but it does have limitations. The sample size (10 SCCE patients for the single-cell analysis) is relatively small, which is understandable given how rare SCCE is, but it means we need to be cautious about generalizing the findings too broadly. Also, validating these findings experimentally in lab models is tricky because good experimental models for SCCE are hard to come by.
Despite these challenges, this work is a massive step forward. It provides an unprecedented, high-resolution map of the SCCE ecosystem, revealing key differences from other esophageal cancers and highlighting potential vulnerabilities we didn’t fully appreciate before. It gives researchers and clinicians valuable resources and biological insights to build upon.
Ultimately, this study doesn’t provide all the answers, but it shines a bright light on promising new directions for tackling this aggressive disease. The focus on angiogenesis and the detailed understanding of the cellular landscape and heterogeneity are invaluable steps towards developing more effective, perhaps even personalized, treatments for patients facing Small Cell Carcinoma of the Esophagus. It’s a tough fight, but studies like this give us real hope.
Source: Springer