Beating the Odds: How Rituximab Tackled Stubborn Leukemia MRD
Hey there! Let’s chat about something pretty fascinating happening in the world of fighting leukemia. Specifically, a tricky type called Acute Lymphoblastic Leukemia (ALL). Now, ALL can be a real challenge, especially in adults. We’ve gotten better at treating it, thanks to borrowing some intensive strategies from pediatric care, but it’s still a complex beast. Things like your age, the specific characteristics of the leukemia cells, and whether tiny traces of the disease – what we call minimal residual disease (MRD) – stick around after treatment, all play a huge role in how things turn out. And honestly, MRD is one of the biggest headaches. If it’s still there, even at super low levels, it means the leukemia could come back.
The CD20+ Twist
Adding another layer of complexity, about 30-50% of B-cell ALL (B-ALL) cases have this marker on their cells called CD20. And historically, that’s been linked to poorer outcomes. But, we’ve found that adding a drug called rituximab, which is an antibody that targets CD20, to the initial chemotherapy can actually improve things for these patients. That’s a win!
When Standard Treatments Fall Short
Despite these advances, we still face tough situations, especially when the leukemia comes back or doesn’t fully respond (what we call relapsed/refractory or R/R). We’ve got newer tools like blinatumomab, inotuzumab ozogamicin (InO), and even CAR-T cell therapies, which have shown promise. But even with these, a guaranteed cure isn’t always on the table. And for some patients, things like other health issues make intensive treatments or a stem cell transplant (HSCT), which is often the best shot at a cure, just not possible.
A Unique Case Emerges
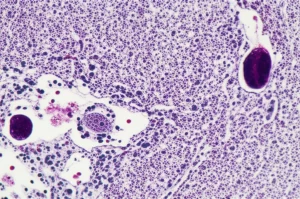
Here’s where things get really interesting. I came across this report about a patient, a 54-year-old woman, who had Philadelphia-negative (Ph-) CD20+ B-ALL. She had some significant health challenges, including heart failure and liver issues, which meant a stem cell transplant wasn’t an option for her. She went through standard intensive chemotherapy, which got her into remission, but that pesky MRD was still detectable. Then, she received blinatumomab, and *poof*, the MRD was gone! That was great news. She continued with treatment, but later on, the MRD popped back up. She got blinatumomab again, and again, the MRD cleared. But then, frustratingly, it reappeared a second time, albeit at a low level.
Trying Something Different: Rituximab Solo
So, she’d been through the standard intensive chemo and had blinatumomab twice, but the MRD just wouldn’t stay away, and a transplant wasn’t an option. What do you do in a situation like that? This is where the doctors made a bold move. Given that her leukemia was CD20+, they decided to try rituximab, but this time, *by itself*, as a monotherapy. This was considered an “off-label” use – meaning it wasn’t the standard approved way to use the drug in this specific scenario, but it made sense scientifically.

The Remarkable Result
She started receiving rituximab courses. And guess what? After just one course, her MRD levels started dropping. After a few more cycles, her MRD became undetectable (< 10^-4), and it stayed that way! Treatment had to be paused because she developed a severe case of COVID-19 that required intensive care – a scary time, I'm sure. But even after stopping rituximab, at her last check-up 15 months later, her MRD was *still* undetectable.
Why This Case is a Big Deal
This patient had a lot of factors stacked against her: age, other health problems, persistent MRD after initial chemo, and MRD relapses after blinatumomab, plus being ineligible for a transplant. These are all things that usually point to a poor prognosis. We know MRD is a critical marker – getting rid of it is strongly linked to better survival. Blinatumomab is great for clearing MRD in many cases, as shown in studies like the BLAST trial, but it doesn’t work for everyone, and failing blinatumomab is a tough spot to be in. Other new therapies like InO and CAR-T are being explored for MRD persistence, but they don’t always achieve 100% MRD eradication, and they come with their own challenges.

We’ve seen rituximab work wonders when combined with chemotherapy upfront for CD20+ B-ALL – it’s become standard practice in many places because it significantly improves outcomes. There have also been a couple of reports of rituximab being used in specific situations (like in Ph+ ALL or combined with chemo in pediatric R/R cases) to help clear MRD or bridge to transplant. But using rituximab *alone* to eradicate MRD in a Ph- CD20+ adult patient who had already failed intensive chemo and blinatumomab, especially when transplant wasn’t an option? As far as we know, this is the first documented case of its kind.
Looking Ahead
This single case report is incredibly exciting. It provides what we call a “proof of concept.” It shows that rituximab, even by itself, *can* be effective in clearing MRD in this specific, difficult-to-treat situation. It highlights a potential lifeline for patients who, like this woman, have limited options left, particularly those who can’t undergo a stem cell transplant. Of course, one case isn’t enough to change practice overnight. We desperately need larger studies and prospective clinical trials to validate this finding and see if rituximab monotherapy could become a go-to strategy for MRD eradication in Ph- CD20+ B-ALL patients who haven’t responded to or can’t receive other treatments. But for now, this story gives us a really promising signal and definitely warrants further investigation. It’s a reminder that sometimes, revisiting existing therapies in new ways can open up unexpected possibilities!
Source: Springer