Tiny Helpers from Your Blood: How Exosomes Speed Up Diabetic Foot Ulcer Healing
You know, diabetes is tough. It affects so many parts of your body, and one of the really nasty complications can be diabetic foot ulcers (DFUs). These aren’t just little cuts; they’re chronic wounds that are incredibly difficult to heal. They can lead to serious infections, long hospital stays, and sadly, sometimes even amputation. It’s a huge burden, not just for the person suffering but for their families and the healthcare system too.
We’ve got ways to treat them, sure – cleaning them up, taking pressure off, managing blood sugar, antibiotics if needed. But honestly, they often take forever to close, and they have a frustrating habit of coming back. It feels like the body’s own repair crew just isn’t getting the job done properly in these cases. So, scientists and doctors have been looking for something better, something that can really kickstart that healing process.
Enter PRP: Your Body’s Own Repair Kit
One promising approach that’s been getting a lot of buzz is Platelet-Rich Plasma, or PRP. Maybe you’ve heard of it being used in sports injuries? It’s pretty neat – it comes straight from *your* own blood. They take a sample, spin it down in a special machine, and concentrate the platelets. These platelets are like tiny little factories packed with growth factors, proteins, and other goodies that signal cells to grow, divide, and rebuild tissue. Because it’s from you, there’s no worry about your body rejecting it.
PRP has shown some real potential in speeding up wound healing, even in those stubborn diabetic ulcers. We’ve seen studies suggesting it can reduce healing time and wound size. It seems to give that sluggish repair crew the boost they need.
The Body’s Cleanup and Construction Crew: Macrophages
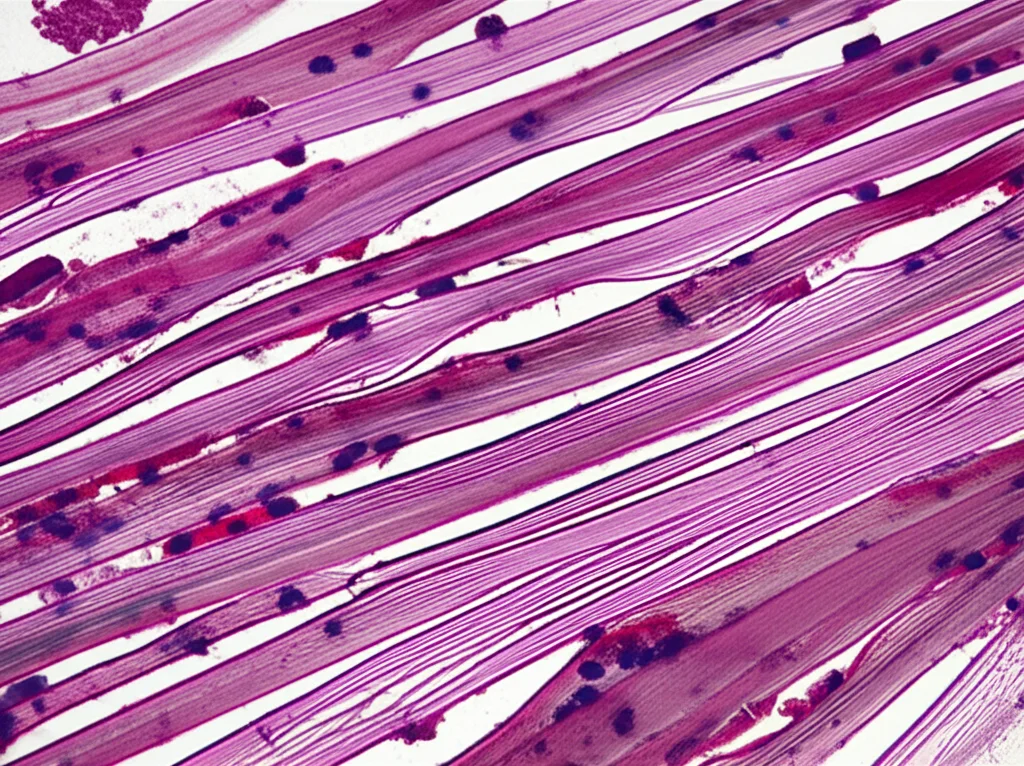
Now, healing is a super complex process, and a key player in it is a type of immune cell called a macrophage. Think of macrophages as the body’s versatile workers. In the early stages of healing, they act like a cleanup crew (we call this the M1 type) – clearing out damaged tissue and fighting off any potential infection. But then, they need to switch gears and become the builders (the M2 type), promoting new tissue growth, laying down collagen (the scaffolding of new skin), and helping new blood vessels form.
In DFUs, this switch often doesn’t happen properly. The cleanup crew (M1) hangs around too long, causing chronic inflammation, and the builders (M2) don’t show up in sufficient numbers. This imbalance is a big reason why these ulcers get stuck and don’t heal.
Discovering the Secret Messengers: PRP-Derived Exosomes
But wait, there’s more! Recent research has shown that a lot of the good stuff PRP does might be thanks to tiny little packages it releases called exosomes. Think of exosomes as microscopic messenger bags, carrying proteins, genetic material, and other signals from one cell to another. They’re like the ultimate biological communication system. Scientists wondered if the healing power of PRP could be bottled up, in a way, by isolating these exosomes.
So, in this study, we decided to take a really close look. We wanted to see exactly how PRP (specifically in a gel form, which is often used for wounds) and these PRP-derived exosomes (PRP-Exos) work their magic on diabetic ulcers, especially focusing on how they influence those crucial macrophage crews.
What We Found: PRP-Gel Gives a Helping Hand
First off, we looked at patients with DFUs who were treated with PRP-gel made from their own blood. And yes, it worked! We saw clear improvements in wound healing – the ulcers got smaller and started closing up, which is fantastic news for anyone dealing with this.
To really understand *how* it was working, we used a diabetic mouse model. These mice develop wounds that behave a lot like human DFUs. We treated their wounds with either a control solution or PRP-gel. Just like in the human patients, the PRP-gel significantly sped up healing in the mice. We saw better re-epithelialization (new skin forming) and more organized collagen deposition, which makes the new tissue stronger.
And when we looked at the immune cells in the mouse wounds, we found something interesting. The PRP-gel reduced the number of neutrophils (another type of immune cell involved in early inflammation) and, importantly, it influenced the macrophages. In the early stages, it seemed to calm down the pro-inflammatory M1 macrophages, and as healing progressed, it boosted the numbers of the pro-healing M2 macrophages. It was like PRP-gel was helping the macrophage crew transition from cleanup to construction.
The Exosomes: Even More Powerful Messengers?
Next, we isolated the exosomes from PRP. We used fancy techniques like transmission electron microscopy (TEM) and nanoparticle tracking analysis (NTA) to see them and measure their size (they’re tiny, around 100nm!) and western blotting to confirm they had the right molecular markers for exosomes. Yep, we successfully captured these little messengers.
Then came the exciting part: comparing the effect of PRP-gel versus the isolated PRP-Exos on diabetic wounds in mice. And wow, the PRP-Exos group showed *significantly* faster healing than the PRP-gel group. The wounds closed up quicker, new skin formed better, and collagen deposition was improved.
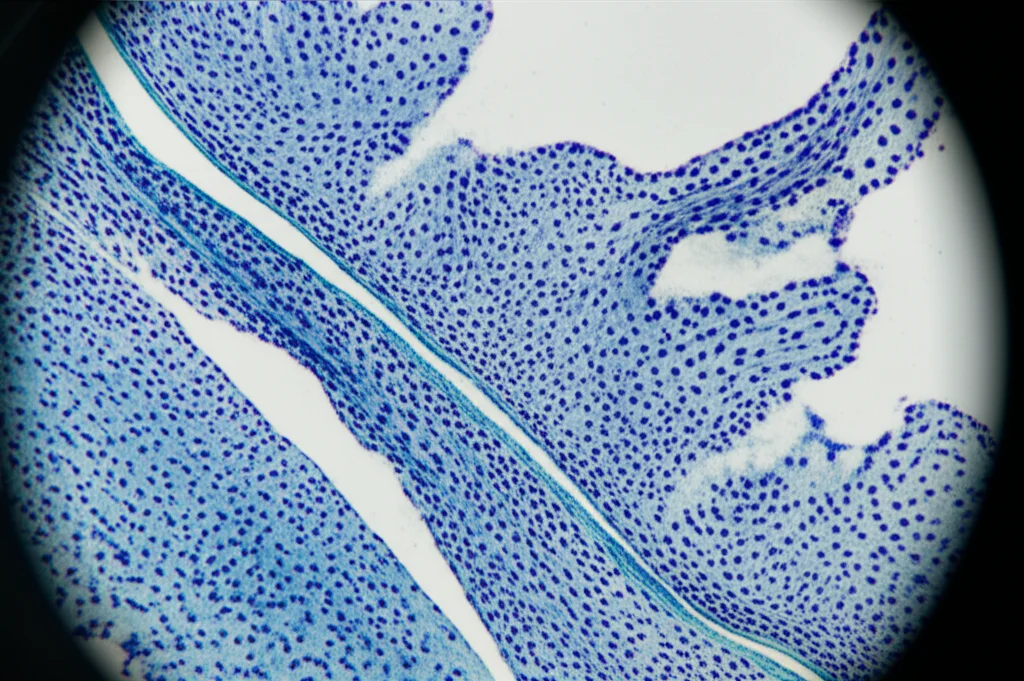
One key thing needed for healing is new blood vessels (angiogenesis) to bring oxygen and nutrients. We looked at markers for new vessels (CD31 and α-SMA) and found that the PRP-Exos were much better at promoting new blood vessel formation compared to PRP-gel. More blood supply means better healing!
The Macrophage Connection: The Key Mechanism
But the real star of the show seemed to be the macrophages. When we looked at the mouse wounds treated with PRP-Exos, we saw a big increase in the number of M2 macrophages compared to the PRP-gel group. This suggested the exosomes were really pushing that macrophage shift towards the healing type.
To confirm this, we did some experiments in the lab with isolated macrophage cells. We saw that when we added PRP-Exos, they effectively stopped the macrophages from becoming the pro-inflammatory M1 type and strongly encouraged them to become the pro-healing M2 type. It’s clear these exosomes are carrying powerful signals that tell macrophages exactly what to do to help the wound heal.

Wrapping It Up: A Promising Future
So, what’s the big takeaway from all this? Our study provides strong evidence that both PRP-gel and, even more effectively, PRP-derived exosomes can significantly accelerate the healing of diabetic foot ulcers. The key mechanism appears to be their ability to regulate the inflammatory environment and, crucially, promote that essential shift in macrophage polarization from the damaging M1 type to the healing M2 type.
This is really exciting because it gives us a solid scientific basis for using PRP and PRP-Exos as potential therapies for DFUs. It’s not a magic bullet yet, and there’s always more research needed – like understanding the exact molecules in the exosomes doing the work and testing this in larger, more diverse groups of patients. We also wonder if combining exosomes with other therapies, like stem cells or advanced dressings, could be even better.
But for now, this study gives us a really strong hint that harnessing the power of these tiny messengers from our own blood could be a game-changer in helping those stubborn diabetic foot ulcers finally heal. It’s a hopeful step forward in improving the lives of people living with diabetes.
Source: Springer