Ultrasound to the Rescue: Checking Muscle Health in Critically Ill Kids
Hey there! Let’s chat about something super important when kids get really, really sick and end up in the intensive care unit (PICU). You know, these little fighters are going through a lot, and one sneaky problem that pops up early on is muscle wasting. It’s like their muscles just start to shrink, and sadly, that can make things tougher for them.
Traditionally, checking muscle health in these tiny patients can be tricky. They might be swollen, or just too unstable for complicated tests. But guess what? There’s a pretty neat tool that’s becoming a real game-changer right at the bedside: Point-of-Care Ultrasonography, or POCUS for short. Think of it as a portable ultrasound machine that doctors can use quickly and easily.
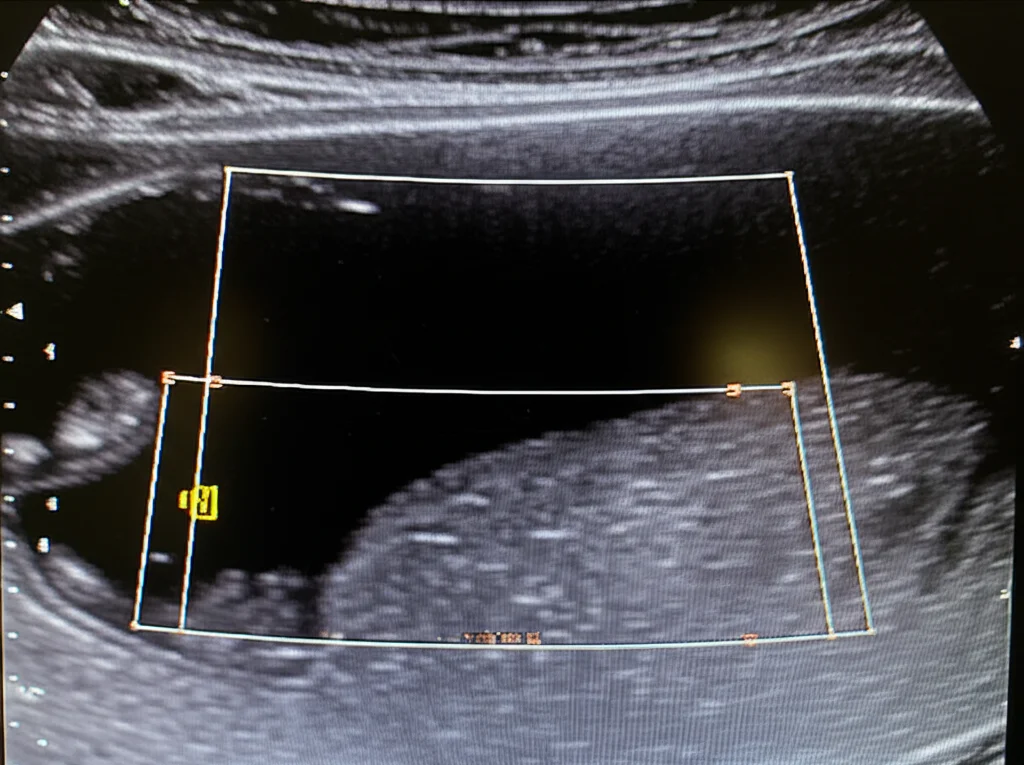
This study I stumbled upon is all about using POCUS to look specifically at the thickness of the quadriceps femoris muscle – that’s the big muscle on the front of the thigh. Why the quadriceps? Well, it’s a big one and easy to get to, even when kids are tucked up in bed in the PICU. The idea was to see if measuring this muscle thickness could help us figure out how well-nourished these kids are when they first arrive and track how things change over their first week.
The Study Setup: Peeking at Tiny Thighs
So, a bunch of clever folks decided to take a closer look. They ran a study involving 55 critically ill children, all hooked up to mechanical ventilation, ranging in age from just 2 months old all the way up to 14 years. They were admitted to a PICU in Cairo.
The plan was simple but smart: use POCUS to measure the thickness of the quadriceps muscle on Day 1 (when they arrived), Day 3, and Day 7. They took a few measurements each time and averaged them out. They were careful to use the same technique and even had a specialist radiologist doing the measurements to keep things consistent.
They also collected tons of other info – things like how sick the kids were (using scores like PRISM and STRONGkids, which helps assess nutritional risk), what they were being fed and if they were hitting their calorie goals, how long they needed the ventilator, and sadly, who made it and who didn’t. They wanted to see if changes in muscle thickness were linked to any of these factors.
What We Found: Muscle Matters!
And guess what they saw? Muscle *melting* away, sadly. Over just the first week in the PICU, the average quadriceps muscle thickness decreased by a noticeable 16.4%! That’s a significant loss in such a short time.
It turns out, if these little fighters weren’t getting enough fuel – specifically, if they failed to achieve at least two-thirds of their target caloric requirements during that first week – they significantly had more muscle wasting. This really highlights how crucial nutrition is right from the get-go.
The study also found that muscle wasting was significantly correlated with several other things:
- Higher STRONGkids score (meaning higher nutritional risk on admission).
- Higher PRISM score (meaning more severe illness on admission).
- Older age (though the median age was quite young in this group).
- Use of inotropes (medications to support blood pressure).
- Certain diagnoses on admission.
- Some lab results like low white blood cell count, low platelet count, prolonged PTT, positive sputum culture, elevated CRP, and elevated serum creatinine.
Interestingly, muscle wasting *didn’t* seem linked to things like sex, initial weight/height measurements, vital signs on arrival, history of chronic diseases or surgeries, developmental stage, supplements used before admission, dialysis, or the use of sedatives or steroids during the PICU stay.

But here’s the really big deal, the one that makes you sit up and pay attention: Muscle wasting was significantly correlated with mortality risk. Yes, losing muscle mass early on was linked to a higher chance of not surviving. It was also linked to how long the kids needed to be on the mechanical ventilator. This suggests that tracking muscle thickness could potentially help predict which kids are at higher risk.
When they crunched the numbers to see what factors *independently* predicted muscle wasting, they found that achieving nutritional goals in the first week and having a positive sputum culture were key independent factors. Another analysis also pointed to the PRISM score and calorie intake as independent predictors.
The percentage of muscle wasting was actually pretty good at helping tell survivors from non-survivors, with a sensitivity of 100% and specificity of 41% at a certain cutoff. The overall ability to discriminate was statistically significant.
Putting It in Context: How Does This Stack Up?
Now, you might wonder, is this study the only one talking about this? Not at all! Other researchers have also used ultrasound to look at muscle changes in critically ill patients, both adults and kids. Some studies in children have also reported significant muscle loss in the first week, similar to the 16.4% seen here. For instance, one study saw a 14% loss, and another reported about a 10% decrease. Some even noted a daily loss rate.
However, it’s not a completely uniform picture across all studies. A couple of studies didn’t find significant muscle wasting in the first few days or even found muscle thickness to be stable. This could be due to differences in the patient groups, how the studies were done, or maybe even subtle muscle activity preserving thickness initially.
The challenge of getting enough nutrition into these kids is well-known. This study’s finding that not meeting calorie goals was linked to muscle wasting aligns with some other research, which even quantified how much muscle size declined for each percentage point decrease in energy intake. But again, a couple of studies didn’t see this link between calories and muscle thickness. Science, right? Sometimes the picture isn’t perfectly clear across different studies.
Using tools like the STRONGkids score to assess nutritional risk is standard practice, and this study confirmed that a higher score was indeed correlated with muscle wasting, just like other research has shown. In adults, a similar score (NUTRIC) has also been linked to muscle wasting.
The high mortality rate in this study (60%) reflects the severity of illness, as indicated by the high PRISM scores. The correlation between high PRISM and STRONGkids scores and muscle wasting, as well as mortality, fits with the understanding that sicker and more nutritionally vulnerable kids are at higher risk. It makes sense – if your body is already struggling and then you start losing vital muscle mass, things get tougher.
Interestingly, this study didn’t find a link between muscle wasting or mortality risk and the total length of time spent in the PICU, which differs from some other findings. But it *did* find a strong link between muscle wasting, mortality risk, and the duration of mechanical ventilation. This connection between ventilation time and poor outcomes is also seen in other studies, especially in developing countries where resources might be more stretched. Getting adequate nutrition is often highlighted as a way to potentially reduce ventilation time and hospital stays.
Why This Matters: The Takeaway
So, what’s the big picture here? This study adds more weight to the idea that muscle wasting is a real and rapid problem for critically ill children in the PICU. It happens fast, within the first week, and it’s clearly linked to not getting enough nutrition.
But more importantly, it shows that this simple, bedside POCUS measurement of quadriceps muscle thickness isn’t just a neat trick; it’s a potentially valuable tool. It can help doctors quickly assess nutritional status and, crucially, it seems to be correlated with serious outcomes like mortality and how long a child needs breathing support.
This really emphasizes two things:
- The importance of getting nutrition into these kids promptly and effectively. Hitting those calorie goals early on seems to make a difference in preserving muscle.
- The utility of using POCUS serially – checking muscle thickness regularly – as an easy way to monitor how a child’s body is coping and potentially flag those at higher risk.
A Quick Note on Limitations
Of course, no study is perfect, and the researchers were upfront about a few things. They didn’t measure the muscle’s cross-sectional area or look at its texture (echogenicity), which some other studies have done and found changes in. They also didn’t specifically track the effect of fluid balance, although other research suggests moderate fluid shifts might not impact thickness much. And since the same radiologist did all the measurements, they couldn’t assess how much results might vary between different people using the ultrasound. These are all things future studies could explore.

Wrapping It All Up
Wrapping it all up, it seems like this little ultrasound trick, POCUS, is a fantastic, easy-to-use tool right there in the PICU. It helped show a significant loss of quadriceps muscle thickness in critically ill kids during that crucial first week. This muscle loss was tied to not getting enough food and, worryingly, to increased mortality risk and longer times on the ventilator.
So, the message is clear: let’s get those calories in, and let’s keep an eye on those muscles with POCUS. It could be a simple way to help these brave kids get through their toughest days.
Source: Springer







