Cracking the Code: Predicting Pancreatic Cancer Surgery Success
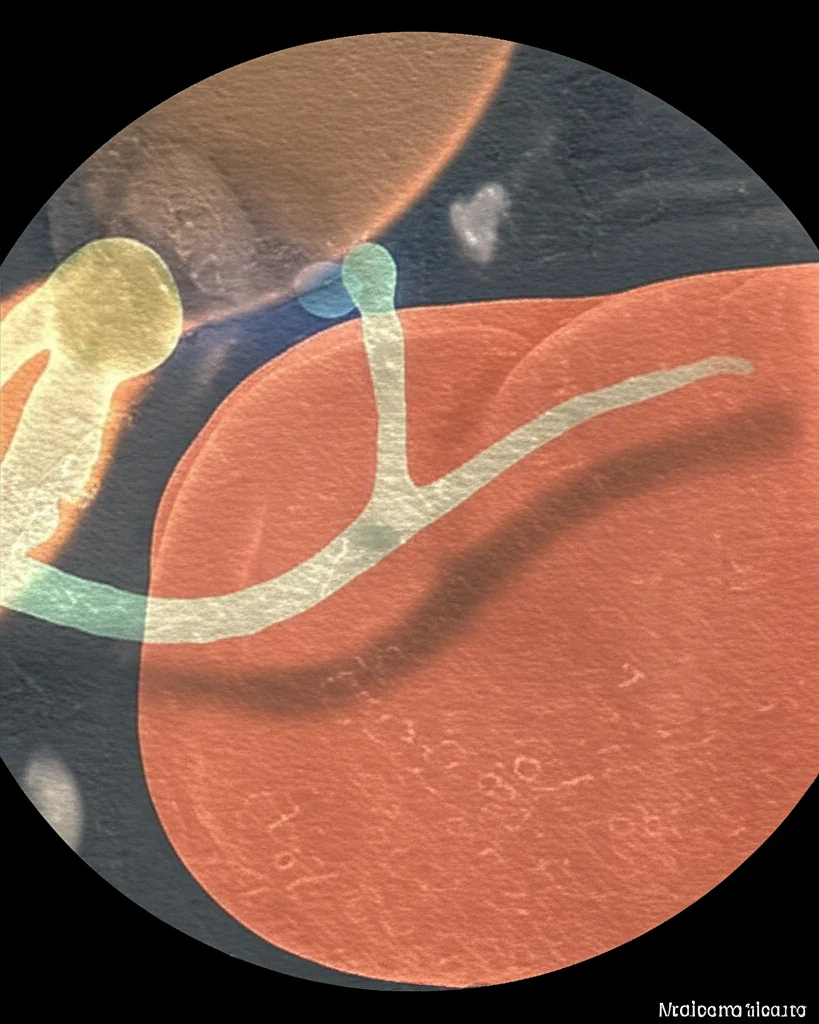
Hey there! Let’s dive into something really important and, frankly, a bit of a tough nut to crack in the world of medicine: pancreatic cancer. We’re talking specifically about those cases where the tumor is close to vital blood vessels – doctors call these “borderline resectable” (BR) or “locally advanced” (LA) pancreatic ductal adenocarcinoma (PDAC).
Now, for these patients, the go-to strategy often involves hitting the tumor with chemotherapy first, usually a powerful regimen known as FOLFIRINOX. The big hope is that this treatment will shrink the tumor or make it less aggressive, opening the door for surgery. Surgery, you see, is currently the *only* real shot at a cure for pancreatic cancer. But here’s the tricky part: figuring out *who* will actually benefit from surgery *after* the chemo. It’s not always clear just by looking at standard scans.
The Prediction Puzzle
Predicting surgical success in BR and LA PDAC after chemotherapy is notoriously difficult. Why? Well, pancreatic tumors often trigger a dense, scar-like reaction around them called the desmoplastic reaction. This can make it super hard for doctors to tell on a standard CT scan whether the tumor is truly invading those crucial blood vessels or if it’s just tangled up in scar tissue. Most patients might show “stable disease” on scans based on standard criteria (like RECIST), which doesn’t necessarily mean the treatment isn’t working on a deeper level.
So, doctors are often left making tough calls. If the tumor hasn’t clearly grown and a certain blood marker (CA 19-9) has gone down, they might propose surgical exploration just to give the patient a chance at a cure. But surgery for pancreatic cancer is a major undertaking, with potential complications. Wouldn’t it be amazing if we could be much more accurate about predicting who will truly benefit?
Current approaches consider things like the tumor’s anatomy, biological markers, and the patient’s overall condition (the A-B-C approach), but they still don’t give us the precision we need. Resection rates after chemo vary wildly in studies, partly because of how patients are selected and where the surgery happens. We need a better way to pick the right candidates.
Enter the PeRFormanCe Trial
That’s exactly what the PeRFormanCe trial is all about! It’s a multicenter, prospective study – meaning it’s happening right now across several hospitals and they’re following patients forward in time. The main goal? To get way better at predicting surgical resectability in BR and LA PDAC patients treated with FOLFIRINOX.
How are they planning to do this? By bringing in some seriously cool, cutting-edge tools:
- Radiomics: This is like getting superpowers for looking at medical images (CT and MRI). Instead of just what the human eye can see, radiomics uses complex computer analysis to extract tons of data from the scans – details about texture, shape, and patterns that might hold clues about the tumor’s biology and how it’s responding to treatment.
- Liquid Biopsy e Multi-omics: This is a game-changer because it’s minimally invasive – just a blood draw! Liquid biopsy lets us look for tiny bits of tumor material (like cell-free DNA or RNA) floating in the blood. “Multi-omics” means they’re not just looking at one thing, but combining insights from different levels – genomics (DNA changes), methylomics (DNA modifications), transcriptomics (RNA activity), and proteomics (protein levels). This gives us a much deeper look at the tumor’s molecular fingerprint and how it’s behaving.
The big idea is that by combining these advanced imaging and molecular insights, we can build a more accurate prediction model than ever before.

How the Trial Works (The Plan)
Patients joining the study have newly diagnosed BR or LA PDAC and are starting FOLFIRINOX chemotherapy. They’ll receive cycles of chemo (up to 12 cycles total). Before starting, they get baseline scans (CT and MRI) and blood drawn for the liquid biopsy stuff.
After every four cycles of chemo, they’re re-evaluated. Now, here’s a crucial point: the decision about whether a patient is ready for surgical exploration is made by a team of experts (the multidisciplinary oncologic meeting) using the *current standard of care*. This means they look at the clinical picture, the standard scans (CT, MRI), and the CA 19-9 levels.
Meanwhile, the trial team is *also* collecting the advanced radiomics data from the scans and running the multi-omics analysis on the blood samples. But – and this is important for the trial’s design – this new, fancy data *doesn’t* influence the decision for *this specific patient* in real-time. Why? Because the goal is to *develop* a prediction model, not to test one that doesn’t exist yet. They need to see what actually happens (was surgery possible? what was the outcome?) and then look back at the radiomics and multi-omics data to see what patterns predicted that outcome.
If the expert team decides surgical exploration is feasible based on the standard criteria (no clear progression, CA 19-9 down in LA cases), the patient goes to surgery. The final decision on whether the tumor can be completely removed (resected) is made by the surgeons during the operation, looking directly at the tumor and surrounding vessels and often using frozen tissue samples.
What Are They Measuring?
This trial is looking at a lot of different things to understand the full picture. The main thing they want to know (the primary endpoint) is the accuracy of predicting surgical resection using these new tools.
But they’re also tracking a bunch of other really important outcomes (secondary endpoints):
- Overall survival and how long patients live without the cancer coming back (disease-free survival).
- How often they achieve a complete (R0) or nearly complete (R1) removal of the tumor.
- How the tumor tissue looks under the microscope after treatment (histopathological response).
- Any complications after surgery.
- Patient-reported outcomes, like quality of life and health economics (because treatment cost and how patients feel are super important!).
- And, of course, the core of the translational research: identifying those specific markers in the radiomics and multi-omics data that predict who will do well and who won’t.
The study plans to include 45 patients who are selected for surgical exploration after NACT. This number was calculated to give them enough confidence in their estimate of how well the multi-omics data can predict *unresectable* tumors (they’re aiming for a high specificity of 90%).

The Science Behind the Scenes
Think of radiomics as turning medical images into mineable data. Every pixel, every texture, every shape characteristic is analyzed by algorithms. It’s like finding hidden patterns the human eye might miss, patterns that could correlate with how aggressive a tumor is or how it’s responding to chemo.
Liquid biopsy is equally fascinating. Tumors shed cells, DNA, RNA, and proteins into the bloodstream. By analyzing these tiny fragments, we can get a real-time snapshot of the tumor’s biology without needing a tissue biopsy. Multi-omics takes this further by looking at multiple types of these molecules simultaneously, building a comprehensive profile.
The trial will use statistical methods, including logistic regression, to see if the patterns found in the radiomics and multi-omics data before and after chemo can predict whether surgery is successful and how the patient will fare long-term. All this data is being carefully collected and managed in a secure electronic system.
Patients are followed closely after surgery, with regular check-ups, blood tests (including CA19-9), and scans to monitor for recurrence. Quality of life questionnaires are also given at multiple points throughout the treatment journey.
Why This Matters So Much
Ultimately, the goal of the PeRFormanCe trial is to improve patient care. Pancreatic surgery is complex and carries risks. If we can get better at identifying which patients are truly likely to benefit from it *after* chemotherapy, we can avoid putting patients through unnecessary procedures if their tumor biology suggests a poor outcome regardless of surgery.
By understanding the tumor’s biology more deeply through radiomics and multi-omics, doctors can potentially:
- Select patients for surgery with greater confidence.
- Personalize treatment strategies based on a patient’s unique tumor profile.
- Monitor treatment response more effectively.
- Potentially improve survival rates and quality of life.
This study represents a really exciting step forward in trying to crack the code of pancreatic cancer. It’s about moving beyond just looking at the tumor’s size on a scan and delving into its deeper biological secrets to make smarter, more personalized treatment decisions.

We’re hopeful that the results from this trial will provide the tools needed to build a more accurate prediction model, ultimately leading to better outcomes for patients facing this challenging disease.
Source: Springer