Cracking the Code: Our New Immune-Stromal Signature to Predict Ovarian Cancer Prognosis
Hey everyone! Let’s talk about something incredibly important but often shrouded in complexity: ovarian cancer (OC). It’s a tough one, and we’ve been working hard to find new ways to understand it better and, hopefully, improve how we can predict what’s next for patients. So, grab a cup of tea, and let me walk you through some exciting developments we’ve been a part of!
Ovarian Cancer: The Silent Challenge
Ovarian cancer, unfortunately, has a bit of a notorious reputation. It’s one of the deadliest cancers for women globally. Just to give you an idea, by 2023, we were looking at over 300,000 new cases worldwide. That’s a huge number! The tricky part is that OC is often a silent disease in its early stages. Symptoms can be vague, and we don’t have super-effective screening methods for catching it early. This means that, sadly, about 75% of women are diagnosed when the cancer is already at an advanced stage, which makes the five-year survival rate pretty grim.
Even with advances in treatments like combination chemotherapy, targeted therapy, and intraperitoneal chemotherapy, there’s another hurdle. While around 80% of patients initially respond well to treatment, many eventually face chemotherapy resistance and the cancer comes back. This is why finding ways for early detection and better intervention is so crucial – it’s all about improving quality of life and survival chances.
Why We Need Better Crystal Balls for OC
One of the big challenges with ovarian cancer is its heterogeneity. That’s a fancy word meaning it can be very different from one patient to another. This variability contributes to treatment failures and not-so-great prognoses. So, there’s a real urgent need to develop a reliable prognostic model. Think of it as a better crystal ball that can help us understand a patient’s likely journey, tailor clinical interventions more effectively, and ultimately, improve outcomes. We want to move towards more personalized medicine, and for that, we need better tools.
Diving into the Tumor Microenvironment (TME)
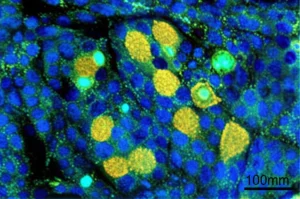
Now, let’s talk about where the cancer lives – the tumor microenvironment, or TME. It’s not just the cancer cells we need to worry about; it’s the whole neighborhood! The TME is a complex mix of cancer cells, the stuff that holds tissues together (extracellular matrix), immune cells, and various molecules. It plays a massive role in how ovarian cancer progresses.
Immunotherapy, especially with immune checkpoint inhibitors (ICIs), has been a game-changer in cancer treatment. But for ovarian cancer, which is known for being quite immunosuppressive, the results have been a bit mixed. While some patients with recurrent or metastatic OC do benefit, the overall response rate is around 13-18%. This tells us we need to understand the immune landscape within the TME much better.
The immune cells and stromal cells (like connective tissue cells) in the TME are getting a lot of attention. Figuring out what these cells are doing can give us big clues for diagnosis and prognosis. That’s where our research journey began. We wanted to explore the relationship between immune and stromal components in the TME and how they affect patient outcomes.

We used a cool tool called the “ESTIMATE” R package. This helps us calculate scores for the amount of immune and stromal cells in OC samples based on gene expression data. We looked at data from The Cancer Genome Atlas (TCGA), a fantastic resource.
Our Hunt for Prognostic Clues: Genes, Genes, Genes!
So, armed with these immune and stromal scores, we went hunting for genes! We analyzed OC expression data and found 1,667 differentially expressed genes (DEGs). These are genes whose activity levels were significantly different when we compared samples with high versus low immune and stromal scores. That’s a lot of genes, right? It’s like finding a treasure map with many potential X-marks-the-spot.
We didn’t stop there. We wanted to see which of these genes were common to both immune and stromal score changes. We found 761 such genes (595 were more active, and 166 were less active). When we looked at what these genes do (using GO and KEGG pathway analyses – tools that tell us about gene functions and pathways), we saw they were heavily involved in things like:
- Immune cell activation
- Extracellular structure organization (the scaffolding around cells)
- Cytokine interactions (how cells talk to each other, especially immune cells)
- Cell adhesion (how cells stick together)
This confirmed that these genes are indeed busy in the immune and structural aspects of the TME. It was a good sign that we were on the right track!
Introducing Our 6-Gene Superhero: The Risk Model
Okay, from those many genes, we needed to narrow it down to the real key players for prognosis. This is where some clever statistical methods come in, like LASSO Cox regression. It’s a way to pick out the most important genes linked to survival while avoiding overfitting (making a model that only works for the data it was built on but not for new data).
And voilà! We developed a 6-gene risk model. These six genes are:
- ALOX5AP
- FCGR1C
- GBP2
- IL21R
- KLRB1
- PIK3CG
Using the expression levels of these six genes, we could calculate a risk score for each patient. This risk score then allowed us to stratify OC patients into high-risk and low-risk groups. The formula looks a bit like this (simplified): Risk score = (ALOX5AP * its coefficient) + (FCGR1C * its coefficient) – (GBP2 * its coefficient) and so on for the other genes. Some genes add to the risk, and some reduce it, based on their coefficients.
Putting the Model to the Test: Does It Work?
Developing a model is one thing; making sure it actually works is another! We did several checks.
First, we looked at survival. And guess what? Patients in the high-risk group (as defined by our 6-gene signature) had significantly poorer overall survival compared to those in the low-risk group. This was a big thumbs-up for our model.
Then, we used something called an ROC curve analysis to see how well our model could predict survival at 1, 3, and 5 years. The Area Under the Curve (AUC) is a measure of predictive accuracy – the closer to 1, the better. Our model showed strong predictive accuracy, with an AUC of 0.744 for overall survival prediction in the TCGA cohort. This told us that our risk score, derived from this immune and stromal signature, could be an independent prognostic factor in OC. Pretty cool, right?

We also looked at how the expression of these six genes correlated with each other and with clinicopathological features like tumor stage, recurrence, etc. We found that things like vital status, tumor residual disease, and stage were distributed differently between our high- and low-risk groups. The high-risk group, as expected, had a considerably higher mortality rate.
What About Treatment? A Sorafenib Surprise!
Prognosis is important, but what about treatment? We wondered if our risk model could give us clues about drug sensitivity. Using a computational tool (the “pRRophetic” package), we analyzed sensitivity to various chemotherapeutic agents.
And here’s an exciting finding: patients in the low-risk group (according to our model, which is a bit counterintuitive as often high-risk patients are targeted, but this relates to specific drug mechanisms) showed heightened sensitivity to a drug called sorafenib. Sorafenib is a multi-kinase inhibitor, meaning it blocks several enzymes involved in cancer growth.
To take this a step further, we did some in vitro experiments (lab tests on cells). We used ovarian cancer cell lines (SKOV3 and A2780) and found that sorafenib effectively inhibited their invasion and metastasis (spread). This suggests sorafenib could be a particularly useful drug for a subset of OC patients, and our model might help identify them. We even did some experiments knocking down one of our key genes, ALOX5AP, and saw that it significantly reduced the proliferation of SKOV3 cells.
Beyond the 6 Genes: Understanding the Bigger Picture with WGCNA
To get an even deeper understanding, we used another sophisticated technique called Weighted Gene Co-expression Network Analysis (WGCNA). This helps identify modules of genes that are co-expressed, meaning their activity levels go up or down together, and how these modules relate to clinical traits like our immune and stromal scores.
We found a “turquoise module” of genes that was most highly correlated with the immune score, stromal score, and the combined ESTIMATE score. It was like finding a whole gang of genes working together! From this module, we identified hub genes – the most connected and important genes within the network. This process helped us select 175 genes for further analysis, which eventually led us to our final six through LASSO regression.
Functional analysis (GO and KEGG again) of these hub genes showed they were involved in crucial processes like T cell activation, regulation of lymphocyte activation, and pathways like the PI3K-Akt signaling pathway, which is well-known for its role in tumor progression. This gave us more confidence that we were focusing on biologically relevant players.
Clustering Patients: Not All Ovarian Cancers Are the Same
Using the 175 WGCNA-identified DEGs, we performed consensus clustering on the 306 OC patients. This grouped them into three distinct clusters. Interestingly, patients in cluster 1 tended to have longer survival compared to those in clusters 2 and 3. This further highlighted the prognostic relevance of these immune and stromal related genes and showed that we could potentially subtype OC based on these molecular signatures.
We also looked at the relationship between our final risk score and the ESTIMATE-derived scores. We found a negative correlation between the risk score and both the ESTIMATE score and the stromal score. This means that a higher risk score was associated with lower stromal cell presence. The correlation with the immune score wasn’t significant, suggesting a complex interplay. These findings point to how variations in the tumor immune microenvironment can influence the unfavorable prognosis in the high-risk group.

Gene Set Enrichment Analysis (GSEA) also told us that high-risk patients had certain signaling pathways more active, like the Notch, Wnt, and VEGF signaling pathways – all known culprits in cancer progression.
The Nomogram: A Personalized Prognostic Tool
To make our findings even more clinically useful, we developed a nomogram. A nomogram is a graphical tool that doctors can use to predict a patient’s prognosis by combining several factors. We performed univariate and multivariate Cox regression analyses, which confirmed that our risk score was an independent prognostic factor, alongside other clinical factors like age, tumor grade, and tumor residual (how much tumor is left after surgery).
Our nomogram integrated the risk score, grade, and tumor residual. Calibration curves showed good consistency between what the nomogram predicted and what was observed for 1-, 3-, and 5-year overall survival. When we stratified patients based on the total points from the nomogram, those with high scores had the worst prognosis. The ROC analysis for the nomogram showed excellent predictive accuracy, with AUC values of 0.755, 0.7963, and 0.846 for 1, 3, and 5 years, respectively. This suggests our nomogram could be a really reliable tool for predicting overall survival in OC patients.
Validating Our Findings: Across Datasets and in Our Hospital
A model is only as good as its ability to work in different situations. So, we validated our 6-gene risk model in independent GEO datasets (GSE17260 and GSE14764) and the ICGC database. The results held up! Patients classified as high-risk by our model had significantly poorer overall survival (OS) and progression-free survival (PFS) in these external cohorts. The AUC values were also strong, ranging from 0.741 to 0.817. This robust validation across different datasets was super encouraging.
We even applied the model to 49 ovarian cancer patients treated at our own hospital (Cangzhou Central Hospital), using their RNA sequencing results and clinical data. The model showed high predictive accuracy here too, confirming its potential real-world utility.
A Closer Look at Our Six Star Genes
Let’s briefly touch upon what these six genes in our signature do, as they are quite fascinating:
- ALOX5AP (Arachidonate 5-Lipoxygenase-Activating Protein): Involved in inflammation and leukotriene synthesis. Its dysregulation is linked to cancer progression.
- FCGR1C (Fc Gamma Receptor Ia): Plays a role in how antibodies help immune cells kill cancer cells (ADCC) and clear debris (phagocytosis).
- GBP2 (Guanylate-Binding Protein 2): Known for antiviral defense, but also emerging as a player in cancer progression by regulating tumor growth and invasion.
- IL21R (Interleukin-21 Receptor): A key regulator of immune responses, influencing immune cell infiltration and anti-tumor immunity.
- KLRB1 (Killer Cell Lectin-Like Receptor Subfamily B Member 1): Associated with Natural Killer (NK) cell activity, important for innate immunity against cancer.
- PIK3CG (Phosphoinositide-3-Kinase Gamma): Part of the critical PI3K signaling pathway, involved in tumor cell proliferation, survival, and immune evasion.
Understanding these genes helps us see why they might be so important for predicting OC prognosis and potentially for guiding immunotherapy decisions. For example, high expression of IL21R and KLRB1 might suggest a better response to immunotherapy.

What This Means for Patients and Future Research
So, what’s the big takeaway? Our 6-gene TME-related risk model offers a robust way to predict prognosis for ovarian cancer patients. It could be a valuable tool for clinical stratification – helping doctors identify patients who might need more aggressive treatment or closer monitoring. It also opens doors for more personalized treatment approaches.
The drug sensitivity analysis pointing to sorafenib is particularly exciting. It suggests that we can integrate these kinds of immune-related biomarkers with targeted therapies to achieve better outcomes. Perhaps sorafenib could be used in combination with immunotherapies or other treatments.
The Road Ahead: Limitations and Hopes
Of course, every study has its limitations. Ours was retrospective, using publicly available data, which can have inherent biases. We also need more direct experimental validation of how these six genes specifically contribute to therapy resistance or sensitivity in vivo. While our in vitro sorafenib results are promising, they reflect general drug activity, and we didn’t verify if the cell lines aligned with the 6-gene risk profiles, which is a step needed for clinical translation.
External validation in diverse populations and larger, prospective clinical trials are crucial next steps to really establish the model’s generalizability and robustness. Integrating other ‘omics’ data (like proteomics or metabolomics) could make the model even more powerful.
Despite these points, we’re really hopeful! Our study underscores the clinical significance of this six-gene signature. It has the potential to enable earlier risk stratification and better prognostic monitoring for women with ovarian cancer. Higher risk scores point to poorer outcomes, and by digging deeper into the mechanisms these genes control, we might uncover new avenues for personalized treatments.
In conclusion, we believe this work is a significant step forward. It’s all about piecing together the complex puzzle of ovarian cancer, one gene, one pathway, one patient at a time, to hopefully change the landscape of OC management for the better. Thanks for sticking with me through all this science – it’s a journey, but a worthwhile one!
Source: Springer