Unlocking the Secret to Soothing Heartburn: How a Tiny Molecule Fights Reflux Inflammation
Alright, let’s talk about something many of us have probably dealt with at some point: that burning, uncomfortable feeling in your chest. Yep, I’m talking about reflux, or more specifically, reflux esophagitis (RE). It’s basically when stomach stuff splashes back up into your esophagus, causing irritation and, importantly, a whole lot of inflammation. It’s not just annoying; it can lead to more serious problems down the line.
For ages, we’ve known inflammation is a big deal in RE. It’s like the body’s alarm system going haywire because of the acid and bile splashing around. But exactly *how* that inflammation gets triggered and *what* could potentially calm it down has been a hot topic for researchers. That’s where this study comes in, looking at a tiny player with a potentially big impact.
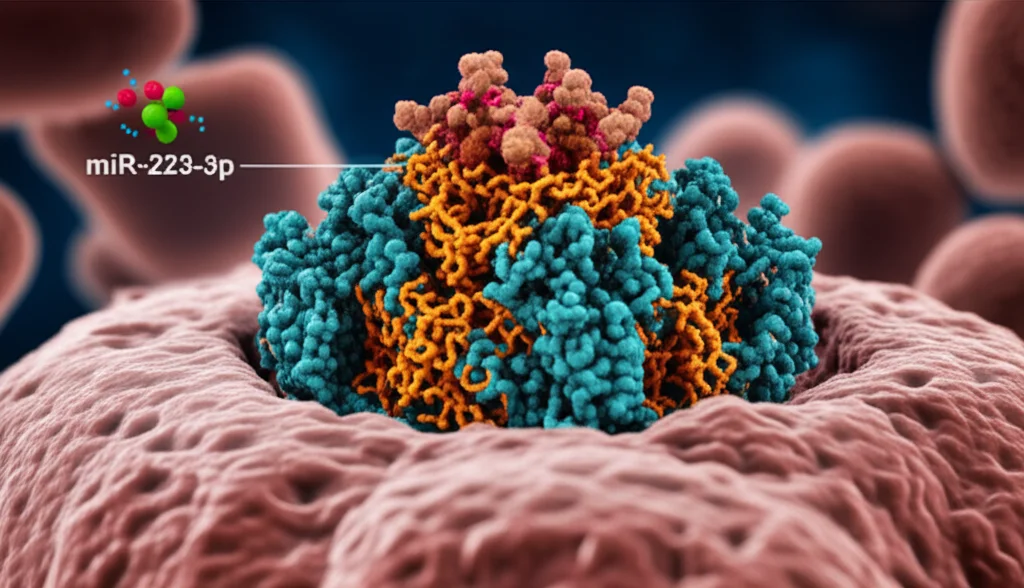
Meet the Players: NLRP3 and miR-223-3p
Think of inflammation like a fire. You need a spark to start it and fuel to keep it going. In our cells, one of the key sparks is something called the NLRP3 inflammasome. It’s a complex little machine that, when activated by irritants (like, say, stomach acid), triggers the release of powerful inflammatory signals. These signals call in the troops, causing damage and discomfort.
Now, enter our other main character: miR-223-3p. This is a type of microRNA, which are basically tiny molecules that don’t code for proteins themselves but act like master switches, controlling when and how much of certain proteins get made. Scientists have found that miR-223-3p seems to have a knack for putting the brakes on NLRP3. It can bind to the genetic instructions (mRNA) for NLRP3 and tell the cell, “Hey, maybe don’t make so much of that NLRP3 right now.”
So, we have RE causing inflammation, NLRP3 being a key driver of that inflammation, and miR-223-3p potentially being able to dial down NLRP3. See where this is going? The big question this study wanted to tackle was: Can miR-223-3p actually help with reflux esophagitis by targeting this NLRP3 inflammasome?
Setting Up the Scene: The Lab Model
To figure this out, the researchers couldn’t exactly give people reflux on purpose (for obvious reasons!). Instead, they used a common trick in science: creating a model in the lab. They took human esophageal cells (called HET-1A cells) and exposed them to a mix of acid and bile salts. This basically mimics what happens during reflux in your esophagus.
And guess what? It worked. These cells started acting a lot like inflamed esophageal tissue in RE. They showed:
- Decreased cell viability (they weren’t as healthy or happy).
- Increased levels of inflammatory signals (like IL-1β and IL-18).
- More cell apoptosis (cells basically committing programmed self-destruction, which is a sign of damage).
- Changes in their cell cycle (how they grow and divide), suggesting things weren’t progressing normally.
This confirmed they had a good lab model to study RE inflammation.
The First Clue: What’s Happening Naturally?
With their RE cell model ready, the researchers first checked the natural levels of our two main players. They found that in the cells exposed to acid and bile (the RE model), miR-223-3p levels were *significantly lower* compared to healthy cells. At the same time, the levels of NLRP3 and its buddies involved in the inflammasome pathway were *significantly higher*.
This is a pretty strong hint! It suggests that when reflux is causing trouble, miR-223-3p gets suppressed, allowing the inflammatory NLRP3 pathway to ramp up. It’s like the body’s natural anti-inflammatory brake is being lifted.
Testing the Theory: Boosting and Blocking miR-223-3p
Okay, so miR-223-3p is low when things are bad. What happens if you *increase* it? The researchers used techniques to artificially boost the levels of miR-223-3p in their RE cell model. They also did the opposite, blocking miR-223-3p to see what would happen.
The results were quite telling:
- When they *overexpressed* (boosted) miR-223-3p, the RE symptoms in the cells got much better. Cell proliferation increased, apoptosis decreased, and the release of inflammatory factors (IL-1β and IL-18) dropped significantly.
- When they *knocked down* (blocked) miR-223-3p, the RE symptoms got worse.
This experiment strongly supported the idea that having enough miR-223-3p is protective against the damage and inflammation caused by reflux.
Confirming the Direct Link: miR-223-3p Targets NLRP3
We suspected miR-223-3p works by targeting NLRP3, but how do you prove they’re directly linked? Scientists use something called a dual-luciferase reporter assay. It’s a clever technique that can show if a microRNA (like miR-223-3p) is directly binding to and affecting the expression of a specific gene’s mRNA (like NLRP3).
And the assay confirmed it! miR-223-3p *does* directly target NLRP3. This means it can directly interfere with the cell’s ability to make the NLRP3 protein.
The Final Proof: Can NLRP3 Undo miR-223-3p’s Good Work?
If miR-223-3p is helping by putting the brakes on NLRP3, then boosting NLRP3 should cancel out miR-223-3p’s benefits, right? The researchers did one more crucial experiment. They took cells where they had boosted miR-223-3p (which we know helps) and then *also* boosted NLRP3.
The results were clear: when both were overexpressed, the protective effects of miR-223-3p were reversed. The cells showed increased apoptosis, worse cell cycle progression, and higher levels of inflammatory proteins and other markers of damage, just like in the original RE model. This pretty much sealed the deal, showing that miR-223-3p works its magic in RE primarily by keeping the NLRP3 inflammasome in check.

So, What Does This All Mean?
This study gives us some really exciting insights. It confirms that the NLRP3 inflammasome is a key player in the inflammatory damage seen in reflux esophagitis. More importantly, it highlights miR-223-3p as a crucial regulator in this process. When miR-223-3p levels are low (as they seem to be in RE), the NLRP3 fire can burn brighter. But boosting miR-223-3p can dampen that fire, protecting the esophageal cells from damage and helping them recover.
This isn’t just academic; it opens up new possibilities. Current treatments for RE often focus on reducing stomach acid. While helpful, they don’t directly address the underlying inflammatory response in the esophageal tissue itself. Finding a way to increase miR-223-3p levels or mimic its effects could offer a completely new therapeutic strategy to tackle the inflammation head-on.
Looking Ahead: The Path to Treatment
Of course, lab studies are just the first step. While these results are promising, there’s still work to be done. We need to see if these findings hold true in living organisms (like animal models) and eventually in humans. Scientists also need to explore the best ways to deliver miR-223-3p or drugs that boost its activity safely and effectively.
Plus, the world of biology is complex! While this study focuses on NLRP3, miR-223-3p likely affects other pathways too, and its role might even change depending on the specific context or stage of the disease. Some previous studies have even shown conflicting results about miR-223-3p levels in RE, suggesting there’s more to learn about its dynamic role.
Despite these complexities, this research provides a really solid foundation. It points to miR-223-3p and the NLRP3 inflammasome as critical players in reflux esophagitis and potential targets for future therapies. Imagine a future where we can treat RE not just by reducing acid, but by also using tiny molecules to calm the inflammation directly. That would be pretty neat!
Source: Springer