Kidney Warriors: PLEX vs. CYC in the Fight Against Lupus Nephritis with TMA
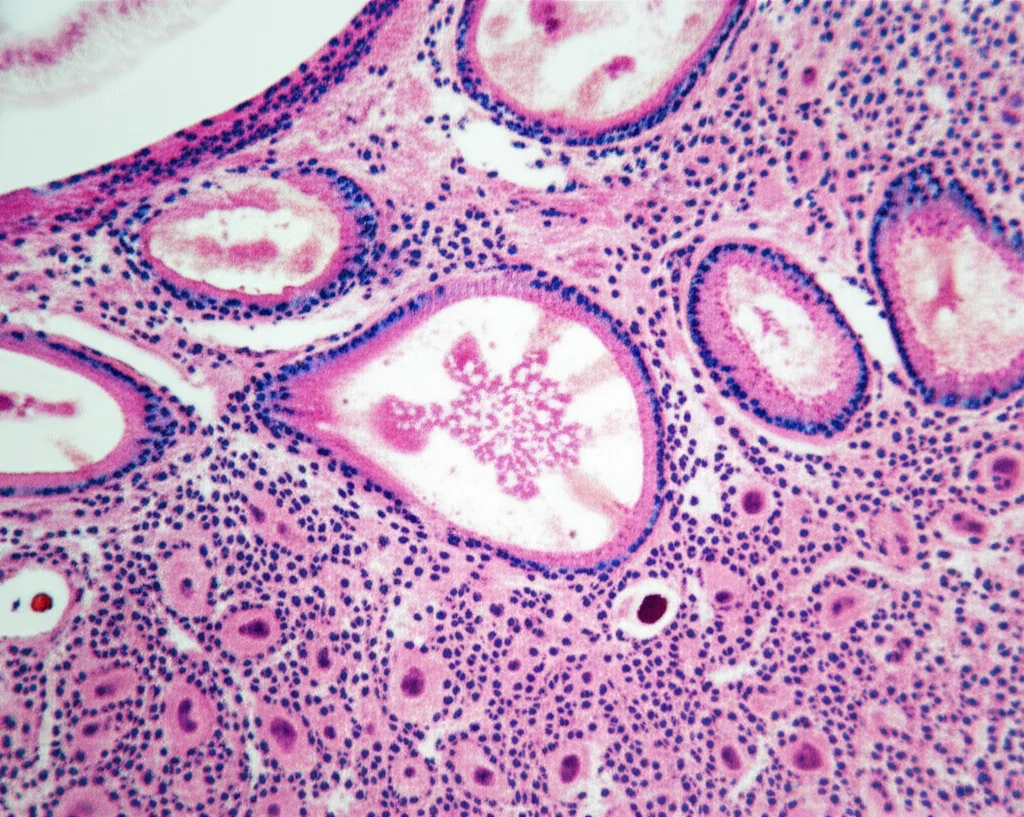
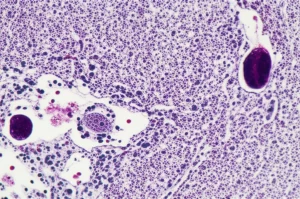
Hey there! Let’s chat about something pretty serious but super important in the world of health, specifically for folks dealing with lupus. We’re diving into a study that looked at a tough complication called Thrombotic Microangiopathy (TMA) when it hits the kidneys alongside Lupus Nephritis (LN). Think of TMA as tiny blood clots messing up the small blood vessels, and when it teams up with LN, which is lupus attacking the kidneys, things get tricky.
Why is this such a big deal? Well, this combo is known for making kidney outcomes worse and sadly, increasing risks. The tricky part is, doctors haven’t had a clear playbook on the *best* way to treat patients facing this specific challenge. So, a bunch of smart folks decided to compare two main strategies: Plasma Exchange (PLEX) and Cyclophosphamide (CYC). They wanted to see which one might offer a better shot at long-term kidney health.
Diving into the Study Details
So, how did they go about this? They did what’s called an ambispective observational study. That’s a fancy way of saying they looked back at records and then followed patients forward. They rounded up 100 patients from Kasr Alainy hospitals at Cairo University who had proliferative LN (that’s classes III or IV, meaning more active inflammation) *and* TMA. All these patients had started treatment with either PLEX or CYC within three months before the study kicked off.
These were all women, with a mean age around 25 – really young to be facing such tough health battles. They followed everyone for a year, keeping a close eye on how their kidneys were doing, how their blood counts looked, and other important markers. They wanted to see who responded best and stayed stable.
The Treatments on Trial
Okay, let’s break down the two main players:
- Plasma Exchange (PLEX): Imagine this like a blood filtering process. They take your blood out, separate the plasma (the liquid part), remove the ‘bad stuff’ that might be causing trouble (like antibodies or faulty proteins), and replace it with healthy plasma or a substitute. In this study, patients in the PLEX group had an average of about 8.5 sessions.
- Cyclophosphamide (CYC): This is a strong immunosuppressant medication. It works by calming down the overactive immune system that’s causing the lupus to attack the kidneys. The CYC group received monthly doses for six months, following a standard protocol.
Both groups also got an initial boost of high-dose steroids, which is pretty standard for severe lupus flares, and then went onto maintenance therapy afterwards (mostly Mycophenolate Mofetil or Azathioprine, depending on availability). It’s pretty amazing that despite how sick these patients were, *none* of them needed dialysis during the study period. That’s a win right there!
Interestingly, the groups weren’t perfectly matched at the start. The PLEX group seemed a bit sicker on some measures, like having higher disease activity scores (SLEDAI) and more signs of TMA activity in their blood and kidney biopsies. The CYC group, on the other hand, started with lower platelet counts and higher levels of protein leaking into their urine (proteinuria). These baseline differences are something to keep in mind when looking at the results.
The Renal Rollercoaster Ride
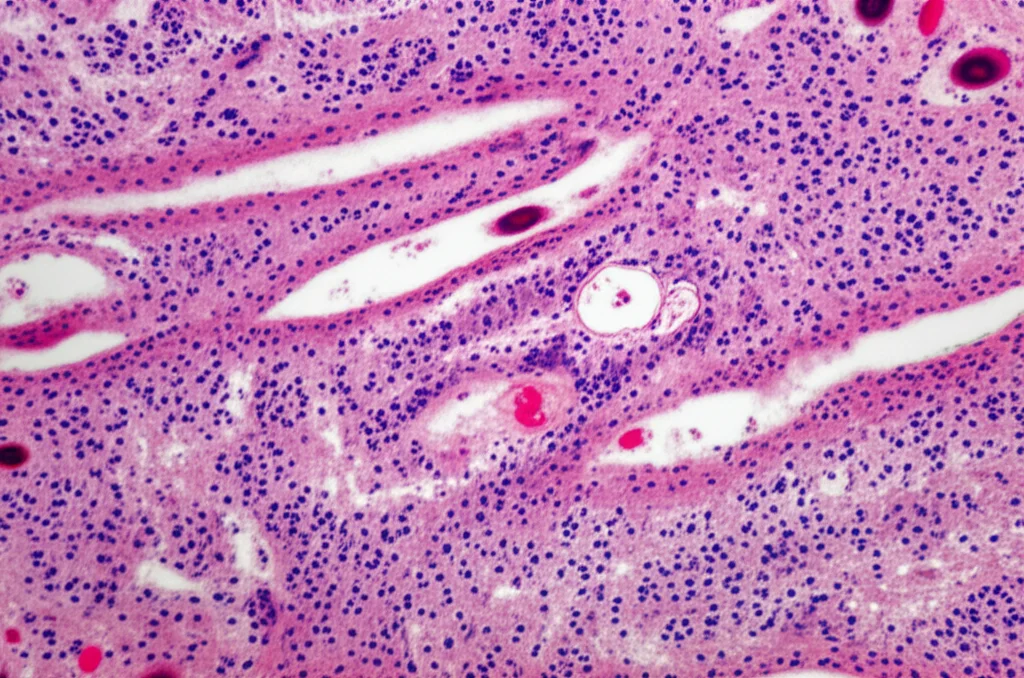
Now, for the main event: how did the kidneys fare? Both treatments helped significantly reduce the amount of protein leaking into the urine over the 12 months. That’s a really important sign of kidney healing.
But here’s where things got interesting:
- Proteinuria: The PLEX group saw a *faster* and *more significant* drop in proteinuria by the 3-month mark compared to the CYC group. And they maintained lower levels even at 12 months.
- Creatinine: This is a measure of kidney function. The PLEX group’s creatinine levels stayed pretty stable throughout the year. The CYC group’s levels were stable for the first 6 months but then *increased* significantly by 12 months. This suggests PLEX might be better at preserving kidney function long-term in this specific situation.
- Overall Renal Response: More patients in the PLEX group hit that early renal response target at 3 months. While both groups improved over time and had similar rates of partial and complete renal response at 6 and 12 months, the stable creatinine in the PLEX group is a key difference pointing towards potentially better long-term kidney health.
Immune and Blood Cell Bounce Back
Beyond the kidneys, they also tracked how the treatments affected the immune system markers and blood counts associated with TMA.
- Complements (C3, C4): These are proteins involved in the immune system, often low in active lupus. Both treatments helped bring these levels up. The PLEX group showed significantly higher C4 levels at 3 and 12 months, and higher C3 levels at 12 months compared to CYC. This suggests PLEX might be better at restoring these specific immune markers.
- Platelets (PLT): Platelets are crucial for clotting, and they drop in TMA. Both treatments were great at getting platelet counts back up. However, the PLEX group saw *faster* and *consistently higher* platelet recovery at all time points compared to CYC.
- LDH: Lactate Dehydrogenase is an enzyme that goes up when red blood cells are being damaged, which happens in TMA. Both groups saw LDH levels drop significantly. Interestingly, the CYC group ended up with *lower* LDH levels at 6 and 12 months than the PLEX group.
So, PLEX seemed to be quicker off the mark for platelets and better for complements, while CYC might have been slightly better at reducing that red blood cell damage marker (LDH) later on.

What Does It All Mean for Patients?
Putting it all together, this study gives us some really valuable insights. It seems both PLEX and CYC, when used alongside steroids and followed by maintenance therapy, can significantly improve outcomes for patients with this tough combination of LN and TMA. That’s good news!
However, PLEX appears to have an edge in the early phase, leading to faster reduction in proteinuria and quicker recovery of platelet counts and some complement levels. The really compelling finding is the difference in creatinine levels at 12 months – stable with PLEX versus increasing with CYC. This hints that PLEX might offer better *long-term protection* for kidney function in these patients.
Why might PLEX be better early on? Well, it physically removes those harmful substances from the blood quickly. This can immediately tackle the TMA process by getting rid of things like problematic antibodies, immune complexes, and factors that damage blood vessels. CYC, being an immunosuppressant, works by suppressing the immune system’s attack over time, which is also effective but perhaps not as immediate for clearing the circulating factors causing TMA.
The study didn’t find any specific patient characteristics (like age, duration of lupus, or disease activity scores) that predicted who would respond better to which treatment, which suggests both options could potentially work for a wide range of patients with this condition.
The Nitty-Gritty (Limitations and Safety Check)
Like any study, this one has its points to consider. It was observational and done at a single center, which means we can’t definitively say PLEX *caused* the better outcomes, just that they were *associated*. There might have been other factors at play. Also, the type of maintenance therapy differed between the groups (more MMF in PLEX, more AZA in CYC), and that could have influenced the long-term results. Plus, some fancy tests that could pinpoint the exact *type* of TMA (like ADAMTS13 levels or specific complement genetic tests) weren’t available, which could have provided more clarity.
On the safety front, both treatments seemed pretty comparable. They tracked complications like infections, disease flares, and changes in white blood cell counts (leukopenia), and there were no statistically significant differences between the groups over the 12 months. Sadly, there were some deaths in both groups, but the rates weren’t statistically different either. This suggests that while these are serious conditions and powerful treatments, neither approach was clearly riskier than the other in this study.
Wrapping It Up
So, what’s the takeaway? This study from Cairo University tells us that for young women battling proliferative lupus nephritis complicated by TMA, both Plasma Exchange and Cyclophosphamide induction therapies, followed by maintenance immunosuppression, can lead to significant improvements in kidney function and blood abnormalities.
However, PLEX showed a clear advantage in achieving faster early responses and, importantly, maintaining stable kidney function (creatinine levels) over the full year, suggesting better long-term kidney preservation. It also seemed better at restoring platelet counts and certain immune markers.
Given these findings, PLEX looks like a really promising option for initial treatment in these complex cases. It seems to hit hard and fast, potentially setting the stage for better long-term outcomes. But, as always in science, more research is needed! The authors rightly call for larger, multi-center randomized controlled trials to really confirm these results and help doctors worldwide decide on the absolute best approach for patients facing this challenging condition.
It’s a reminder that even with tough diagnoses like lupus with kidney complications, research is constantly moving forward, giving us more tools and better hope for managing these conditions and improving lives.
Source: Springer