Beating the Wiggle: How Custom 3D Prints Revolutionized Lung SBRT Testing
Hey everyone! Let me tell you about something pretty cool we’ve been up to. If you’ve ever heard about lung cancer treatment, you know that radiotherapy is a big deal, especially for early-stage cases where surgery isn’t an option. We’re talking about Stereotactic Body Radiation Therapy, or SBRT for short. It’s this amazing technique where we zap the tumor with a really high dose of radiation, but spread out over just a few sessions. The goal? Hit the cancer hard and fast while sparing as much healthy tissue as possible.
But here’s the tricky part, especially with lungs: they move! Every time you breathe, that tumor wiggles around. This respiratory motion is a real headache because it can make the actual radiation dose delivered totally different from what we planned. Imagine trying to hit a tiny moving target with pinpoint accuracy – that’s the challenge.
So, before we can confidently use SBRT on patients, we have to go through this super important process called “commissioning.” It’s basically putting our equipment and plans through rigorous tests to make sure everything is working exactly as it should. And for lung SBRT, these tests *have* to involve a phantom that can mimic breathing motion.
The Problem with Standard Phantoms
Now, there are commercial phantoms out there designed for this, like the QUASAR™ Respiratory Motion Phantom we use. They’re great for simulating the movement. But we ran into a snag when it came to actually *measuring* the dose accurately inside that moving target.
See, with standard setups, if you put a film (which is like a special piece of paper that darkens when radiation hits it, showing the dose pattern) inside the phantom, it moves *with* the simulated tumor. This sounds logical, right? But it creates this effect called “dose blurring.” The film records the dose over the entire path of the tumor’s motion, smearing out the sharp dose lines we expect from our precise SBRT plans. It makes it really hard to verify if our treatment planning system (TPS) is predicting the dose correctly for a moving target.
For point dose measurements (using a tiny detector called an ion chamber to measure the dose at a single spot), the commercial inserts often don’t even put the detector *inside* a moving tumor surrogate. It might just be in the moving “lung” area, which isn’t quite the same thing as measuring the dose right where the cancer is.
We needed a better way to test this, something that would let us see the dose distribution *without* the blurring and measure the dose precisely *within* the moving tumor.
Our Bright Idea: 3D Printing to the Rescue!
That’s where our little project came in. We thought, “What if we could customize our phantom inserts?” And since we’re living in the future, 3D printing seemed like the perfect tool. We decided to design and print our own specialized inserts for the QUASAR phantom to tackle these exact problems.
We came up with two main designs:
- A custom film insert: The goal here was to keep the film *static* relative to the phantom’s main body, even while the simulated tumor part of the insert moved. This way, the film would capture the dose profile at a fixed plane, allowing us to compare it directly to our static TPS calculations without the motion blur mess. We also added features to hold the film securely and protect it from friction damage during the motion.
- A custom ion chamber insert: For this one, we designed a cavity right in the center of a simulated tumor (a little sphere). This tumor part was designed to move with the phantom, so our tiny ion chamber (a CC04 chamber, specifically) would be right in the middle of the action, moving *with* the tumor and measuring the dose delivered to its core.
Pretty neat, right? We figured this would give us a much more accurate picture of what was really happening with the dose delivery in a moving lung.
Building Our Custom Tools
So, we fired up the computer-aided design (CAD) software and got to work. We designed these inserts down to the millimeter, making sure they’d fit perfectly in the QUASAR phantom and hold our detectors just right.
For the 3D printing, we used PLA filament, which is a common and relatively inexpensive material. The trick was getting the density right to mimic lung and soft tissue (like the tumor) on CT scans. We experimented with different infill percentages (how much plastic is inside the print) until we got the right Hounsfield Units (HU) – those numbers you see on CT scans that tell you about tissue density. We ended up using wood-PLA for the lung part and a slightly different infill for the tumor part to get the right HU values.
We printed these bad boys on a standard desktop 3D printer, fine-tuning the settings to make sure they were mechanically accurate and sturdy. The film insert was designed in two halves that screwed together, holding the film firmly in place with cushioning layers. The ion chamber insert also came in halves to easily pop the detector in before screwing it shut, ensuring the chamber was smack-dab in the middle of the moving tumor.
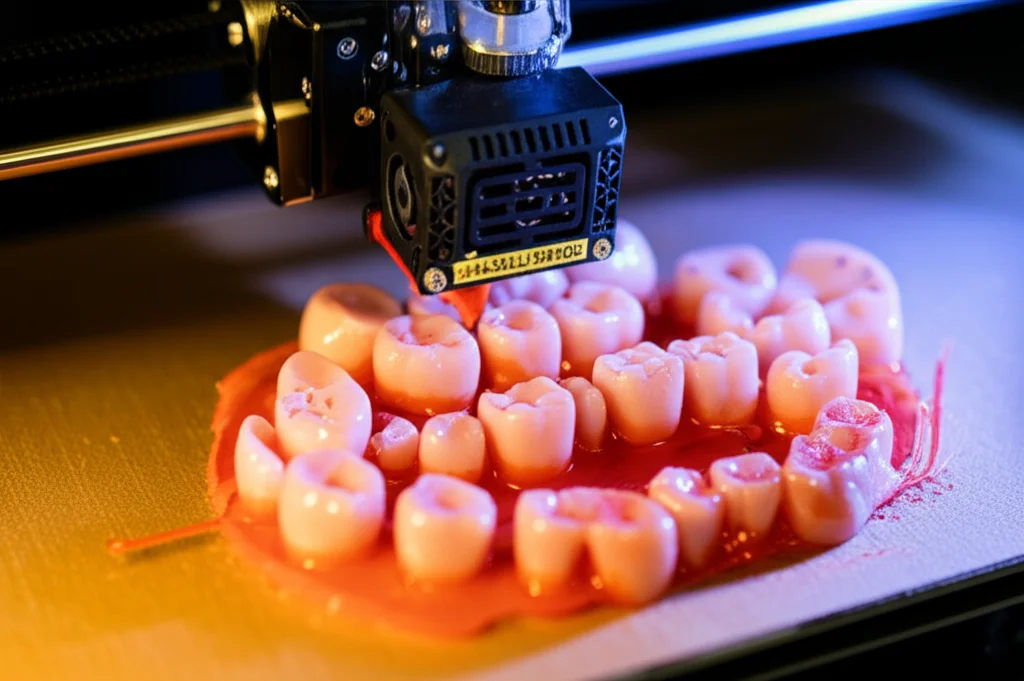
Once printed, we even CT scanned the inserts themselves to double-check their structure and confirm those HU values were spot on. Turns out, they were! The lung part was right in the ballpark for lung tissue, and the tumor part was spot on for soft tissue.
Putting It to the Test (Phantom QA)
With our fancy new inserts ready, it was time for the real tests. We put the inserts with the detectors (film or ion chamber) into the QUASAR phantom and set it up to mimic realistic breathing motion.
We created SBRT plans just for these phantom tests, using our standard treatment planning system (Eclipse with the AcurosXB algorithm). We tested plans using both flattened 6 MV beams and the faster, flattening filter-free (FFF) 6 MV beams, which are often preferred for SBRT because they deliver the dose quicker, potentially reducing the impact of motion *during* the treatment.
We delivered these plans to the moving phantom and then analyzed the results. For the film, we used a technique called gamma analysis, which compares the measured dose pattern to the planned one, checking if they match within certain criteria (like 3% dose difference and 1 mm distance difference). With our static film setup, we saw gamma pass rates over 95% using the strict 3%/1mm criteria. That’s excellent! It showed that our TPS was accurately predicting the dose distribution in a fixed plane, even with the target moving underneath.
For the point dose measurements with the ion chamber *inside* the moving tumor, we compared the measured dose to the dose the TPS predicted for that specific point. We delivered each test plan multiple times and averaged the results. The differences were super small – within 1.9% of the planned dose. This was incredibly reassuring, confirming that our system could accurately deliver the intended dose right to the center of the moving target.
Real-World Practice (Patient Plan QA)
Okay, the phantom tests were a success, proving the concept. But what about actual patient plans? We took anonymized CT data from 20 patients who had previously been treated for lung cancer and created new SBRT plans for them using the technique we were commissioning (free breathing, ITV-based). We used robust optimization techniques in the planning software to minimize the potential impact of motion uncertainties.
We then put these patient plans through our standard departmental quality assurance protocol. This involved delivering the plans to a stationary phantom (a different one, the CIRS thorax phantom) and measuring the dose with film and an ion chamber. This step is crucial to ensure that the *plan itself* is deliverable and the total dose distribution is accurate in a static scenario.
The results were fantastic! The average film gamma pass rates were above 98.8% (using the 3%/1mm criteria), and the point dose measurements were within 2% of the expected values. This confirmed that the SBRT plans we were creating using our established workflow and the robust optimization techniques were accurate and deliverable.

Why This Matters
So, why go through all this trouble with custom 3D prints? Well, it boils down to accuracy and confidence. By using our customized inserts in the dynamic phantom commissioning, we could:
- Mitigate Dose Blurring: Keeping the film static eliminated the motion blur, allowing for a clear, direct comparison with our static TPS calculations. This is much simpler than trying to use complex mathematical models to de-blur the dose.
- Measure Dose at the Target’s Core: Putting the ion chamber *inside* the moving tumor surrogate gave us confidence that we could accurately measure the dose delivered to the actual cancer location.
- Provide a Robust Commissioning Tool: These inserts gave us a reliable way to test our entire SBRT process, from imaging and planning to delivery, specifically accounting for respiratory motion in a meaningful way.
- Offer Flexibility and Cost-Effectiveness: 3D printing allowed us to design inserts tailored to our specific phantom and detectors, and it’s much cheaper and faster than getting custom-made inserts from a commercial vendor every time we need a slight variation (like a different tumor size or chamber type).
This approach effectively addressed limitations we saw in commercially available inserts and previous attempts at 3D printing for this purpose. We could use larger film sizes and avoided the need for manually adding non-printable materials like cork granules, making the process smoother and more reproducible.
Looking Ahead
Now, was this the absolute end of the road? Of course not! This was a single-institutional study, and while the results were incredibly positive and allowed us to confidently commission lung SBRT, there’s always room to grow.
Ideally, we’d love to test even more variations – different tumor shapes, sizes, and more complex, non-sinusoidal motion patterns. That would require printing even more inserts and dedicating significant time to measurements, which wasn’t feasible with our busy clinical workload.
Also, while the QUASAR phantom is great, patient breathing isn’t always a simple up-and-down movement. More sophisticated phantoms that can move in all directions (six degrees of freedom) and even deform like real tissue would be amazing for future testing. And exploring 3D dose measurement techniques (like gel dosimetry or multiple film layers) in a moving phantom is another exciting avenue.
But for now, we’re thrilled with the results. Our custom 3D-printed inserts gave us the robust testing platform we needed to ensure the accuracy and safety of our lung SBRT treatments for patients.
Source: Springer







