Spine Surgery Gets a Close-Up: Ultrasound Inside the Bone
Hey folks! Ever wondered about the nitty-gritty of spine surgery, especially when they’re putting in those pedicle screws? Turns out, getting those tiny holes drilled *just right* is absolutely critical. If a screw goes even a little bit off track, it can cause a whole heap of trouble, from making the spine unstable to, yikes, potentially damaging nerves or even the spinal cord. Nobody wants that!
Naturally, surgeons and engineers are always cooking up new ways to make this process safer and more accurate. We’ve seen everything from fancy 3D-printed guides and robots to augmented reality systems. These are super cool and definitely help reduce errors compared to the old-school ‘free-hand’ method (which, believe it or not, is still pretty common!). But, like most cutting-edge tech, they often come with downsides: they can be expensive, expose patients to radiation (even if it’s reduced), need big surgical cuts, require a steep learning curve, or can even fail if the patient moves during the procedure. They haven’t quite become the standard go-to yet.
Hello, Intraosseous Ultrasound!
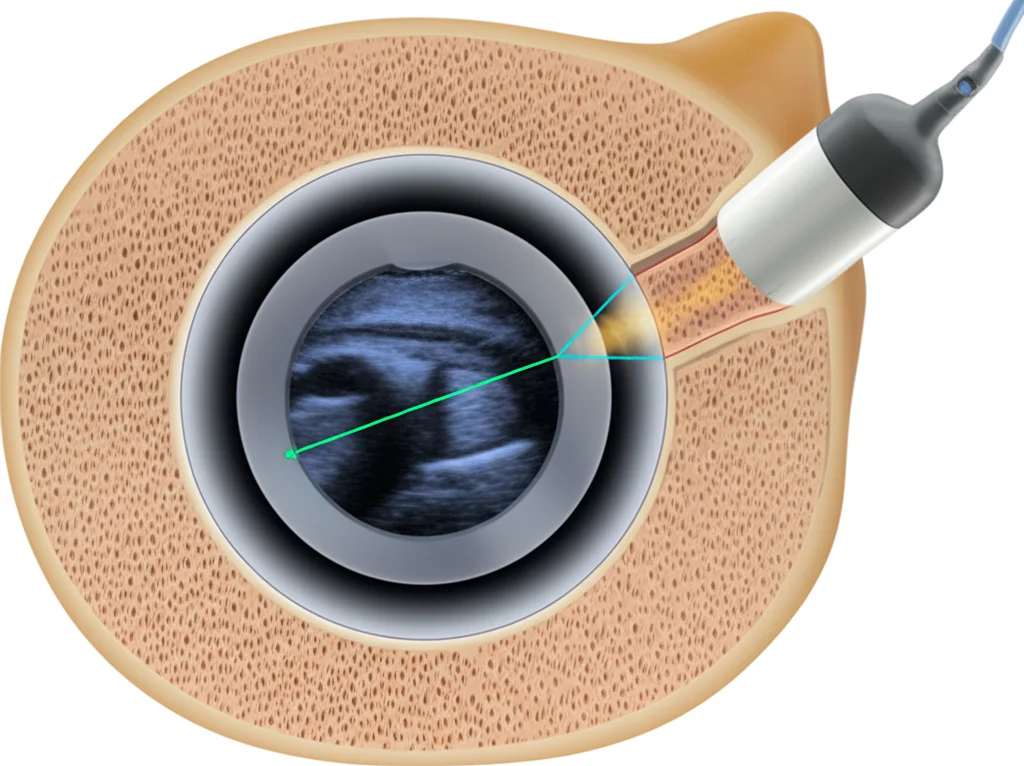
So, what if there was a simpler, more direct way to check things *from the inside*? That’s where a concept called Intraosseous Ultrasound (IOUS) comes in. Think of it as putting a miniature ultrasound probe right inside the bone channel you just created. It lets you see the walls of the hole and the surrounding tissue in real-time. It sounds pretty intuitive, right? And the best part? It doesn’t require a ton of extra equipment or specialized training beyond knowing how to interpret ultrasound images (which, for surgeons, is often part of the deal anyway!).
People have experimented with this before, using probes designed for looking inside blood vessels (called Intravascular Ultrasound or IVUS). They showed it was totally feasible and reliable for checking screw placement, especially in the lower spine. But those IVUS probes had a couple of drawbacks: they were disposable and pricey, and because they were *so* flexible, they could bend inside the hole, potentially distorting the images.

Putting EUS to the Test
This is where our story gets exciting! Someone had a brilliant idea: what about using probes designed for Endoscopic Ultrasound (EUS)? These probes are also mini and flexible, but they have a tip that’s less prone to bending weirdly. Plus, they’re generally lower cost and can be reused. This study was all about seeing if an EUS probe could be used for IOUS *inside* pedicle screw holes, specifically in the thoracolumbar spine, and how accurate and reliable it would be.
So, they set up an experiment using thoracolumbar spine specimens from two goats. Why goats? Turns out their spines in that region are quite similar in size and structure to human ones – a great stand-in for testing! They drilled 76 pedicle screw holes in these spines. Some were placed correctly, but most were intentionally drilled off-center or even breaching the bone cortex (the outer shell) to simulate different types of malposition.
For each hole, they did two things:
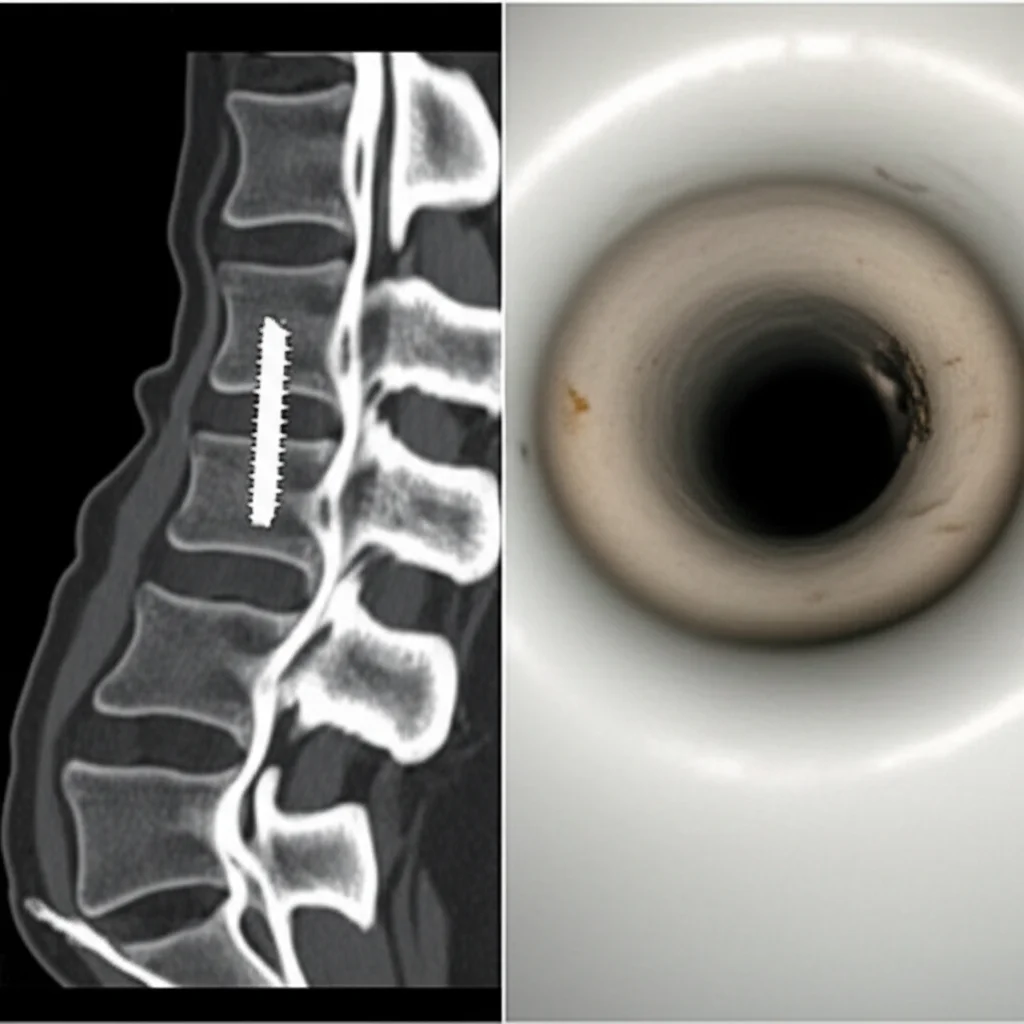
- They inserted a tiny EUS probe (about 2.4mm in diameter) and scanned 360 degrees while slowly pulling it back out. This gave them a stack of ultrasound images for each hole.
- They performed a CT scan of the entire spine specimen. CT is considered the gold standard for seeing exactly where the holes are and if they’ve breached the cortex.
Then, three independent reviewers (two spine surgeons and one sonographer), who had *zero* prior experience with IOUS and didn’t know the CT results, looked at the ultrasound images. Their job was to figure out if the hole was correctly positioned or if there was any malposition or breach. Finally, they compared the ultrasound interpretations to the definitive CT results using some statistical tests.
What the Ultrasound Showed
The results were pretty eye-opening! The CT scans confirmed that out of the 76 holes, only 13 were perfectly placed, while a whopping 63 had some degree of malposition, including many that had broken through the cortex.
Now for the ultrasound part:
- When the hole was perfectly placed, the ultrasound image showed the probe in the center surrounded by a nice, intact, wide ring-like echo from the bone.
- If the hole was slightly or moderately off, the ring would show a deformation or a gap where the cortex was damaged, and you might see echoes from the tissue outside the bone.
- For severely misplaced holes, especially those that broke into the spinal canal, a large part of the bone ring would be missing, and you could even see the echo from the wall of the spinal canal on the opposite side!
Here’s the really impressive bit: *all* the malpositioned holes identified by CT were also correctly identified as malpositioned by the ultrasound reviewers. There were *no false negatives*, meaning they didn’t miss any screw holes that were actually off track! The reviewers also agreed with each other almost perfectly.
There were a few interesting cases that initially caused some confusion:
- Sometimes, even if CT showed the hole was *just* inside the pedicle, the ultrasound showed a slightly enhanced echo near the spinal canal side. This might mean IOUS is even more sensitive to a very thin layer of bone or the tissue right outside it.
- In holes that were close together or intersected, the ultrasound could pick up the wall of the *other* hole, which initially looked like a bone breach (a false positive), but this could be easily identified with a little training.
And the speed? Scanning each hole with the EUS probe took less than 15 seconds! That’s incredibly fast for getting such detailed feedback.
Why This is Exciting
So, why is this EUS-based IOUS technique a big deal?
- Immediate and Reliable: You get real-time feedback on screw hole placement right there in the operating room. The study showed it’s highly reliable for spotting malpositions and breaches.
- Lower Cost: Compared to many advanced navigation systems, EUS equipment is potentially much less expensive, and the probes can be reused.
- Radiation-Free: Unlike CT or C-arm fluoroscopy used in some techniques, ultrasound doesn’t involve ionizing radiation for the patient or the surgical team.
- Suitable for MISS: The flexible, small probe is perfect for minimally invasive spine surgery (MISS) where space is limited.
- Intuitive: The study found that even reviewers with no prior IOUS experience could correctly interpret the images after a brief explanation. The learning curve seems promising.
While it might not have the ultra-high resolution of CT for seeing every tiny bone detail, its ability to clearly show the integrity of the bone channel walls and detect breaches is exactly what you need during screw placement. The slightly lower frequency of the EUS probe (12 MHz) compared to IVUS (20 MHz) actually gives it better penetration into the surrounding cancellous bone, creating that useful “wide ring” image.
Looking Ahead
This EUS-based IOUS technique isn’t necessarily meant to replace *all* other methods, but it looks like a fantastic complementary tool. It doesn’t require the complex setup and potential registration issues of navigation systems. It’s quick, reliable, and radiation-free.
The future possibilities are even more exciting. Imagine a drill bit with a tiny ultrasound transducer built right into the tip! As the surgeon drills the pedicle hole, the ultrasound could provide instant feedback, giving an early warning if the trajectory is drifting off course. This would allow for immediate correction, potentially preventing severe malpositions and injuries before they happen. This experimental study provides solid, reliable data showing that the core concept – ultrasound *inside* the bone channel – is valid and works beautifully. It’s a crucial step in paving the way for those future innovations.
Bottom line? Using EUS probes for intraosseous ultrasound is a really promising, quick, and reliable technique for checking pedicle screw hole placement in spine surgery. It’s a potentially low-cost, intuitive, and radiation-free option that could make these procedures even safer and more accurate. Pretty cool, right?
Source: Springer







