A Triple Threat Against Unresectable Liver Cancer? This Study Says Maybe!
Hey There, Let’s Talk About iCCA
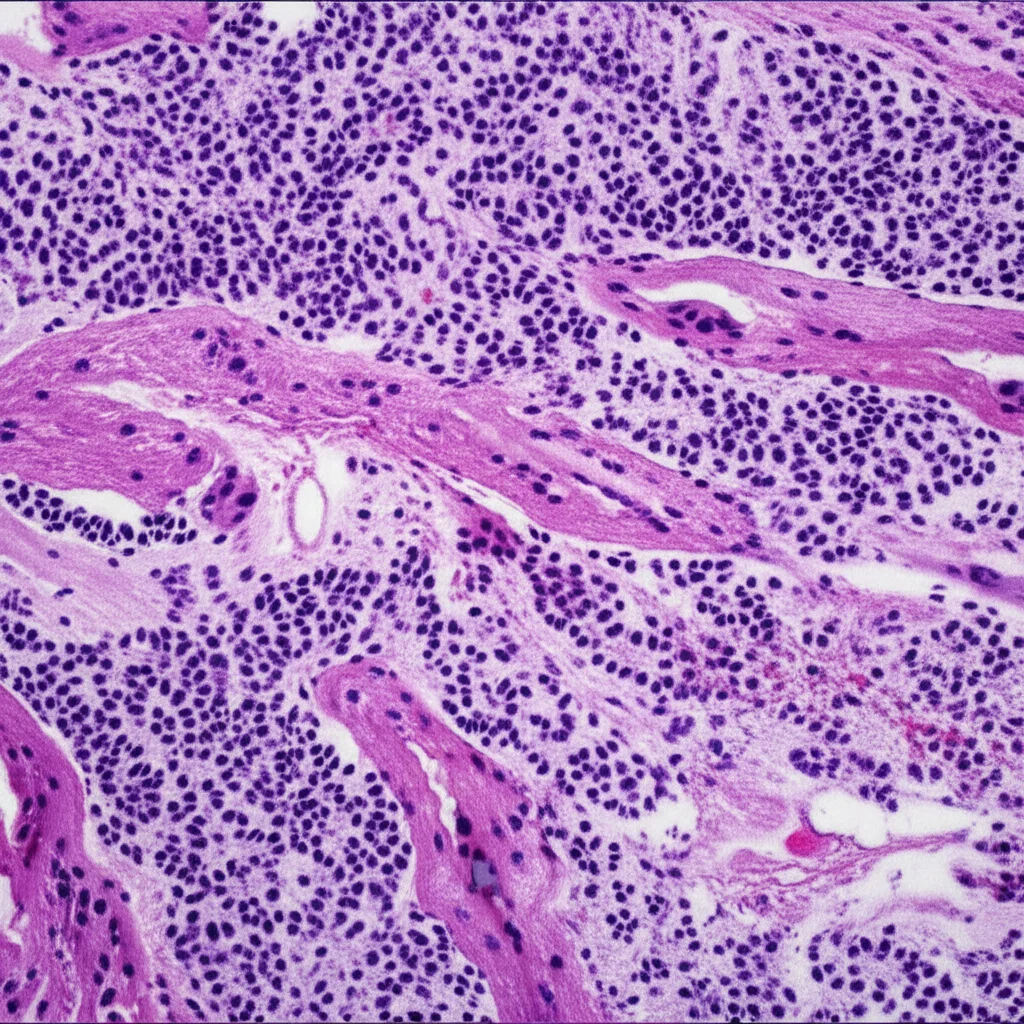
So, you know how sometimes you hear about cancers that are really tough to treat, especially when they’ve decided to make themselves comfortable and aren’t easily removed by surgery? Well, intrahepatic cholangiocarcinoma, or iCCA as the cool kids (and doctors) call it, is often one of those. It’s a type of cancer that starts in the bile ducts inside the liver, and unfortunately, a big chunk of people are diagnosed when surgery isn’t really an option anymore.
When surgery is off the table, the standard game plan usually involves systemic chemotherapy. Think of it as a body-wide attack on the cancer cells. It helps, for sure, but the prognosis, or the outlook, for unresectable iCCA hasn’t been fantastic. We’re talking about a pretty low 5-year survival rate, which tells you we desperately need better options.
Mixing Things Up: A New Combo Approach
Enter the world of combination therapies! Scientists and doctors are always looking for ways to team up different treatments to hit cancer from multiple angles. This study I stumbled upon dives into one such promising combination for unresectable iCCA.
Instead of just standard systemic chemotherapy (SC), they looked at a triple-threat approach:
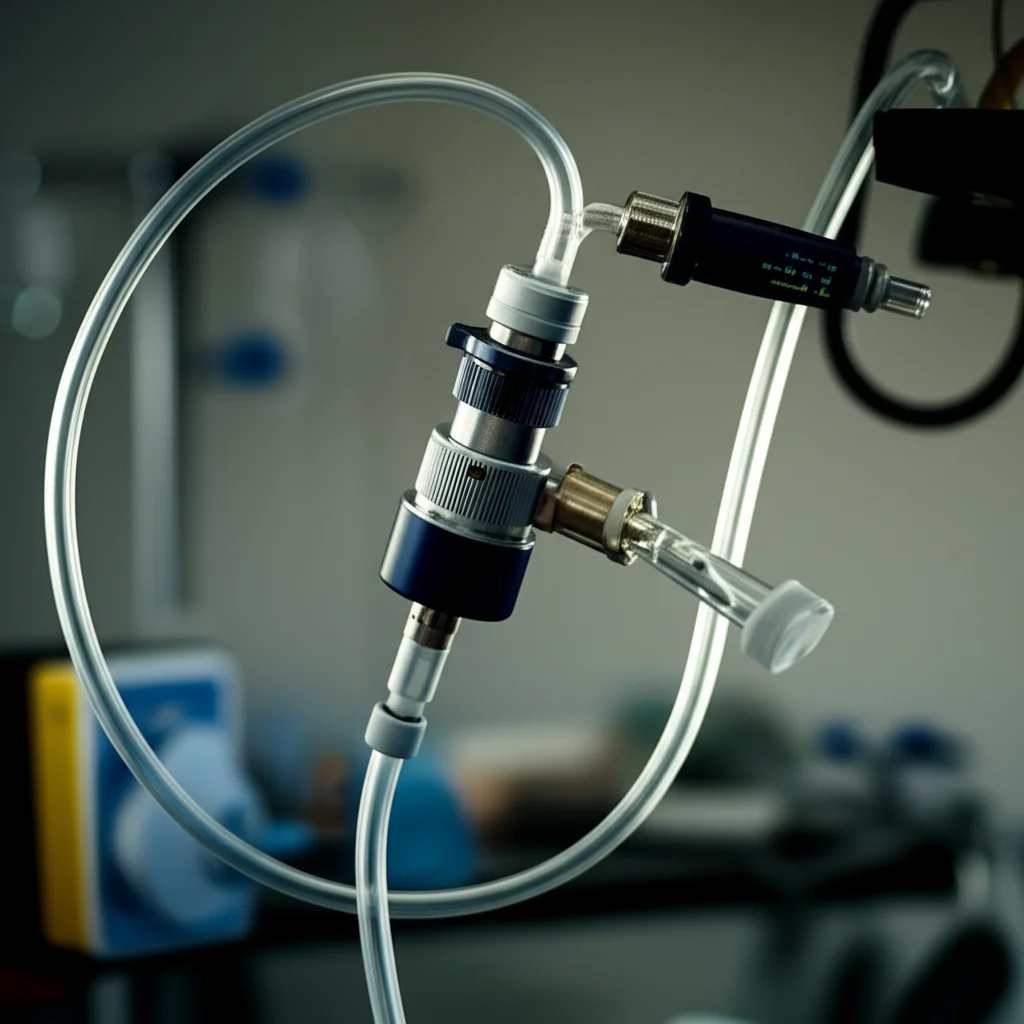
- Hepatic Arterial Infusion Chemotherapy (HAIC): This is pretty neat. Instead of pumping chemo through your whole body (systemic), they deliver it directly into the artery that feeds the liver tumor. The idea is to get a high concentration of the drug right where it’s needed, potentially reducing side effects elsewhere.
- Lenvatinib: This is a targeted therapy. It’s a smart drug that blocks certain signals cancer cells use to grow and build blood vessels (like VEGFR and FGFR pathways, which are often active in iCCA).
- PD-1 Inhibitors: These are part of the immunotherapy gang. They basically take the brakes off your immune system so it can better recognize and attack cancer cells. PD-1 is a protein cancer cells sometimes use to hide from immune cells, and these inhibitors block that hiding mechanism.
So, the big question this study asked was: how does this HAIC + Lenvatinib + PD-1 inhibitor combo stack up against the standard systemic chemotherapy for folks with unresectable iCCA?
How They Figured It Out
To answer this, the researchers looked back at data from patients treated at their center between 2020 and 2022. It was a retrospective study, meaning they analyzed existing records. They included patients who met specific criteria – confirmed iCCA that couldn’t be surgically removed, decent liver function, and a good enough general health score (ECOG 0 or 1).
They had two groups: one got the standard systemic chemo, and the other got the HAIC + Lenvatinib + PD-1 inhibitor combo. To make the comparison fair, even though it wasn’t a randomized trial, they used a statistical method called Propensity Score Matching (PSM). Think of it like trying to find pairs of patients in each group who were as similar as possible in terms of age, tumor characteristics, etc., so they could compare apples to apples. After matching, they ended up with 30 patients in each group.
They then looked at a few key things:
- Overall Survival (OS): How long patients lived.
- Progression-Free Survival (PFS): How long patients lived without the cancer getting worse.
- Objective Response Rate (ORR): What percentage of patients saw their tumors shrink significantly (complete or partial response).
- Disease Control Rate (DCR): What percentage of patients saw their tumors shrink or stay stable.
- Safety: What side effects occurred and how severe they were.
The Big News: The Combo Pulled Ahead
Alright, drumroll please… The results were pretty exciting!
Compared to the standard systemic chemotherapy group, the group receiving the HAIC + Lenvatinib + PD-1 inhibitor combo showed some seriously impressive improvements:
- Overall Survival (OS): The median OS was significantly longer in the combo group (16.91 months) compared to the standard chemo group (11.06 months). That’s a difference of nearly 6 months! While the ultimate mortality rates were similar over the long follow-up, the combo treatment seemed to push those events much further down the road. For patients facing this tough diagnosis, gaining several months of life is a really big deal.
- Progression-Free Survival (PFS): The combo group also had a much longer median PFS (11.17 months) compared to the standard chemo group (5.55 months). More than double the time before the cancer started growing again!
- Objective Response Rate (ORR): The combo group saw a much higher percentage of patients with significant tumor shrinkage (56.7%) compared to the standard chemo group (23.3%). That’s more than double the response rate!
- Disease Control Rate (DCR): Almost everyone in the combo group (93.3%) had their disease controlled (shrunk or stable), versus 70.0% in the standard chemo group.
They also did some fancy statistical analysis and found that being in the standard chemotherapy group was actually a risk factor for *worse* survival outcomes. On the flip side, having a higher hemoglobin level seemed to be a protective factor.
Interestingly, when they looked at subgroups, the combo therapy seemed particularly beneficial for patients with larger tumors (>5 cm), multiple lesions, or tumors involving both lobes of the liver – basically, those with a higher tumor burden. This hints that maybe this local delivery method (HAIC) combined with the systemic agents is especially good at tackling more extensive disease within the liver.
What About Side Effects?
Okay, so it works better, but is it way tougher on the body? The study reported that the side effects were generally comparable and manageable between the two groups.
The most common side effects were things you might expect with cancer treatment, like nausea, abdominal pain, fatigue, and changes in blood counts. The standard chemo group actually had higher rates of leukopenia (low white blood cells), nausea, and vomiting. The combo group did see more hypertension (high blood pressure), which they think is likely due to the Lenvatinib. But overall, there were no major differences in severe side effects, and importantly, *no treatment-related deaths* in either group.
They also noted that the dose of chemotherapy drugs (Gemcitabine and Cisplatin) delivered via HAIC in the combo group was significantly *lower* than the dose given systemically in the standard chemo group, yet it achieved better results. This supports the idea that delivering chemo directly to the liver via the artery is more efficient and potentially less toxic systemically.
Why Might This Combo Work So Well?
The researchers speculate on why this triple therapy might be so effective. It’s likely a case of synergy – the different components working together in ways they wouldn’t alone.
Think about it:
- Lenvatinib can help make the tumor environment more friendly to immune cells.
- HAIC and Lenvatinib can cause damage to the tumor, potentially releasing bits of cancer cells (antigens) that the immune system can then learn to recognize. This process might also make the tumor express more PD-L1, which is the target for the PD-1 inhibitors, essentially making the immunotherapy more effective.
- Combining these different mechanisms might help overcome ways cancer cells develop resistance to single therapies.
It’s like a coordinated attack: one part weakens the tumor’s defenses, another flags the cancer cells for destruction, and the third unleashes the body’s own army.
But, and It’s a Big But…
Now, before we get *too* carried away, the researchers are quick to point out the limitations of their study. And that’s super important in science!
- It was a small study (only 30 patients per group after matching).
- It was retrospective, meaning they looked back at data. This can introduce biases that are hard to control for, even with PSM.
- It was done at a single center. Results might be different elsewhere.
- The standard first-line treatment for advanced biliary tract cancers (which includes iCCA) now often involves systemic chemotherapy *plus* immunotherapy (like Durvalumab). This study compared the combo to *systemic chemotherapy alone*. So, we really need future studies to compare this HAIC-based triple therapy directly against the current standard of systemic chemo *plus* immunotherapy.
- They used different types of PD-1 inhibitors in the combo group, and with the small numbers, it’s hard to tell if one type worked better than another.
So, while the results are really promising and exciting, they need to be confirmed in bigger, better-designed studies – specifically, prospective, randomized clinical trials.

The Takeaway
Despite the limitations, this study gives us a really strong signal. For patients with unresectable iCCA, combining HAIC with Lenvatinib and a PD-1 inhibitor looks like a significantly more effective strategy than standard systemic chemotherapy alone. It led to better tumor control, longer time without the disease progressing, and importantly, longer overall survival, all with manageable side effects.
It reinforces the potential power of combining locoregional therapies (like HAIC) with targeted agents and immunotherapy. It’s a complex disease, and it seems a multi-pronged attack might be the best way forward.
This research is a fantastic step and definitely warrants further investigation. It offers a glimmer of hope and a potential new path for treating this challenging cancer. Keep an eye out for those future studies!
Source: Springer