High-Fat Diet, Thin Air, and Brittle Bones: A Mouse Story
Hey there! Let me tell you about something that really caught my eye. We all know osteoporosis is a big deal, especially as we get older. It makes bones weak and fragile, leading to nasty fractures. But did you know it’s a particularly common problem in places high up, like plateau regions? It seems the thin air, or *hypoxia*, might be part of the story.
Now, add another layer: diet. People living in these high-altitude areas often eat diets that are pretty rich – lots of protein, calories, and fat. This got some researchers thinking: what happens when you combine the stress of thin air with a high-fat diet? Could these two things team up to make bones even weaker? That’s exactly what this study I read about set out to investigate, using mice as their models.
Picture this: mice were split into groups. Some got a regular diet, and others got a high-fat diet (HFD). Both groups lived in a slightly *hypoxic* environment, kind of like being at a moderate altitude (simulating 2000–2200 m). The idea was to see how this combo affected their bones and everything connected to them. And let me tell you, the results were quite telling.
The Weighty Issue: HFD and Body Changes
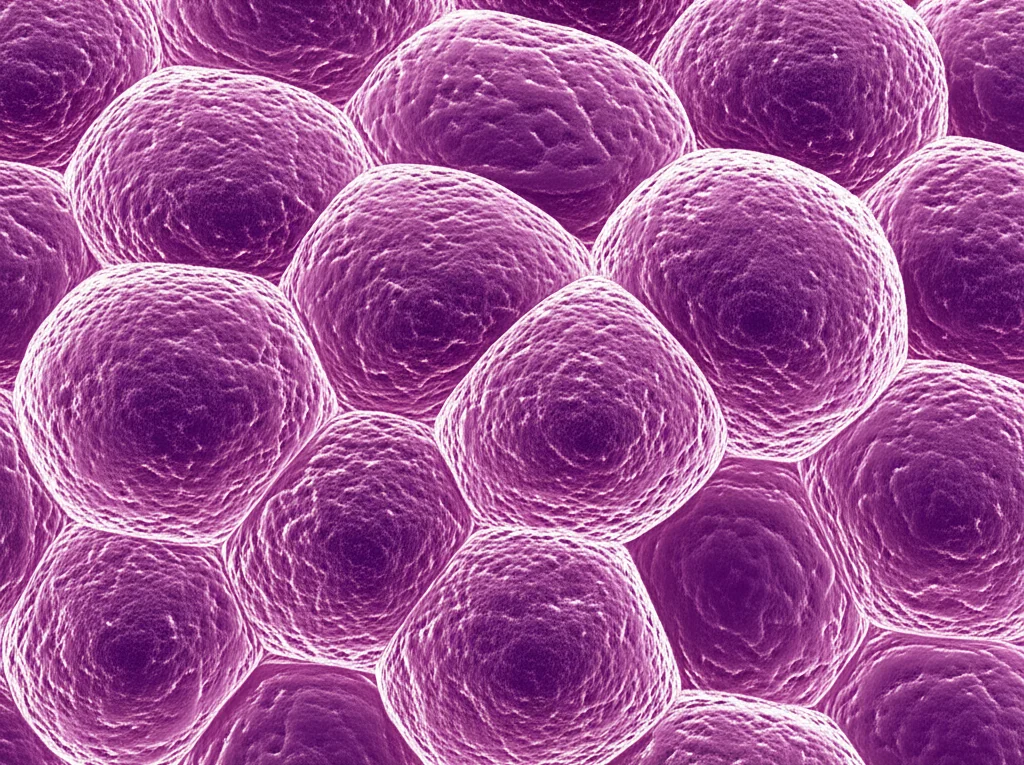
First off, no big surprise here, the mice on the HFD got bigger. Significantly bigger. Their body weight shot up compared to the control group, and not just a little bit – sometimes over 30% heavier! Their Lee’s index, BMI, and body fat percentage also went way up. Pathological exams even showed their fat cells were getting huge and packed with more fat droplets. It’s like they were getting that classic obesity profile, even with the added stress of lower oxygen. This really confirms that the HFD was doing its job in inducing obesity in these mice under hypoxic conditions.
Bone Trouble: What Happens Inside
Okay, so they got heavier. But what about their bones? That’s the crucial part. Using fancy micro-CT scans and looking at tissue samples, the researchers found that the bones of the HFD mice were in rough shape. The delicate network inside the bone (the trabecular bone) was messed up – thinner, sparser, and with wider gaps. The outer layer (cortical bone) was also thinner. Basically, the bone structure was degenerating.
And it wasn’t just the structure. They looked at the cells responsible for bone remodeling – the *osteoblasts* that build bone and the *osteoclasts* that break it down. The HFD group had a significant increase in the number of *osteoclasts*. It’s like the bone-breaking crew went into overdrive.
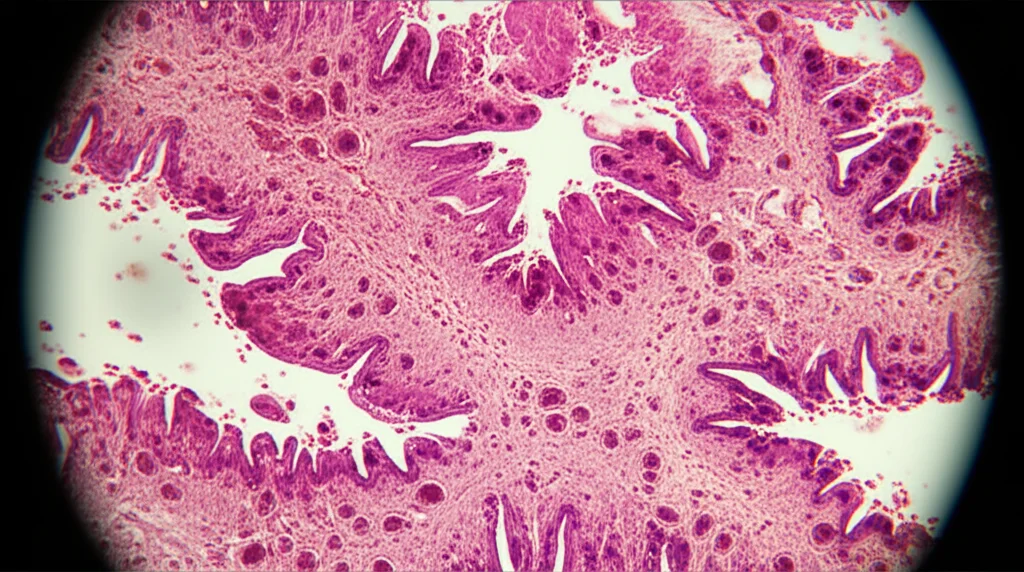
They also checked key markers in the blood, fat, and colon tissues: Alkaline Phosphatase (ALP), Parathyroid Hormone (PTH), and Vitamin D (VD). ALP is usually a sign of bone formation, while PTH and VD are involved in calcium balance and bone resorption. In the HFD group, ALP and PTH levels generally went up, while VD levels went down. This pattern often points towards increased bone turnover with a lean towards resorption, which fits with the increased osteoclasts and structural damage. These findings really hammered home that the HFD was inducing bone metabolic disorders, even under *hypoxia*. It suggests these two factors might be working together to make things worse.
Inflammation Station: Body on Fire
One of the big suspects linking diet and bone health is inflammation. And boy, did the HFD mice have more of it! Pro-inflammatory markers like TNF-α and IL-6 were significantly higher in their plasma, fat tissue, and colon tissue compared to the control group. At the same time, the anti-inflammatory marker IL-10 was lower. It’s like the body was in a state of low-grade fire.
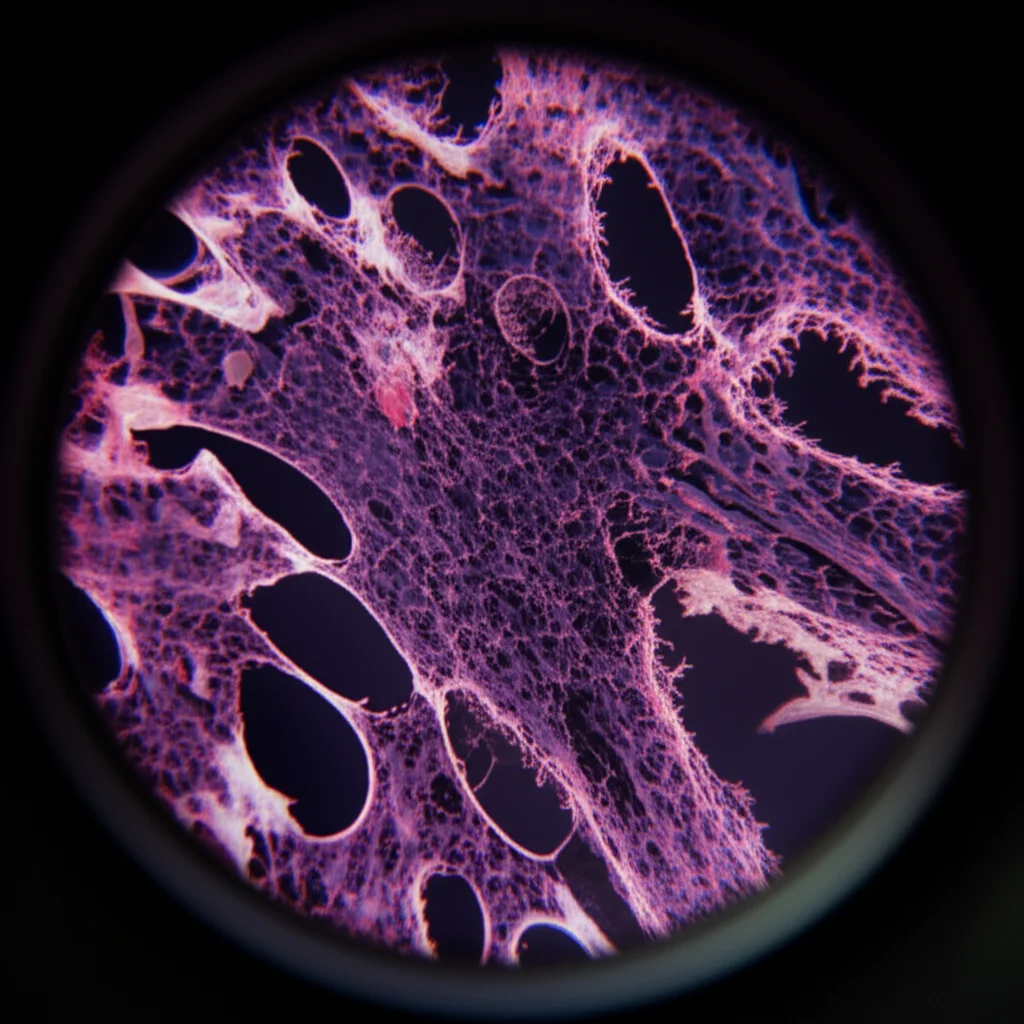
What’s interesting is how this tied back to the gut. The HFD seemed to damage the intestinal lining, leading to increased levels of markers like CALP and LPS, which indicate gut injury. When the gut barrier is leaky, nasty substances (like endotoxins from bacteria) can get into the bloodstream, triggering systemic inflammation that can travel and affect other tissues, including bone. This suggests a vicious cycle where the HFD damages the gut, causing inflammation, which then contributes to bone loss.
Gut Feeling: Microbiota Mayhem
Speaking of the gut, the researchers also took a peek at the gut *microbiota* – the trillions of bacteria living in the intestines. The HFD drastically changed the community structure. Beneficial bacteria, like *Lactobacillus* and *Bifidobacterium*, decreased significantly. These guys are usually good for you, helping with immunity and potentially bone health. On the flip side, bacteria often associated with inflammation, like *Bacteroides* and *Rikenellaceae RC9 gut group*, increased.
This shift in the microbial balance is a big deal because the gut *microbiota* doesn’t just hang out in your intestines; it influences your immune system and produces metabolites that can affect your whole body, including your bones. A gut community leaning towards pro-inflammatory bacteria could easily contribute to the systemic inflammation they observed, further fueling the bone breakdown process.

Metabolite Messengers: The Chemical Signals
The gut *microbiota* also produces metabolites, which are small molecules that can act as signals. The study looked at these and found changes, particularly in metabolites related to histidine metabolism. Two metabolites, Anserine and L-Histidine, were downregulated in the HFD group, while L-Carnosine was upregulated.
Why is this important? Well, histidine metabolism is linked to inflammation, and changes in these metabolites can influence the inflammatory environment. For example, L-Histidine is a precursor to histamine, an inflammatory mediator. Anserine and L-Carnosine, on the other hand, are known to have anti-inflammatory properties.
It seems the body might be trying to fight the inflammation induced by the HFD and *hypoxia* by increasing L-Carnosine. But the downregulation of Anserine and L-Histidine (potentially leading to more inflammatory histamine) suggests the balance is off.
Connecting the Dots: A Complex Network
The researchers didn’t stop there. They used fancy statistical analysis (Spearman correlation and network visualization) to see how all these factors – body weight, bone structure, bone markers, inflammation, gut *microbiota*, and metabolites – were connected. And guess what? They’re all tangled up in a complex network!
This network shows how the HFD and *hypoxia* don’t just act in isolation; they create a cascade of effects. Obesity leads to changes, gut *microbiota* changes influence inflammation, inflammation affects bone cells, and metabolites act as intermediaries in these interactions.
Interestingly, L-Carnosine popped out as a central player, a “key hub” in this network. Its levels were strongly correlated with many other factors, suggesting it plays a crucial role in this complex interplay, possibly as a compensatory anti-inflammatory response. Under the combined stress of *hypoxia* and a HFD, this delicate network gets knocked out of balance, leading to bone metabolic disorders and, ultimately, osteoporosis.

Why This Matters e What’s Next
So, what does this all mean? For people living in high-altitude areas who also consume rich diets, this study provides a scientific basis for understanding why they might be at higher risk for osteoporosis. It highlights that it’s not just one thing, but a combination of environmental (hypoxia) and dietary (HFD) factors working together through a complex pathway involving the gut, inflammation, and metabolism.
Of course, this was a study in mice, and there are limitations. They didn’t have groups just exposed to *hypoxia* alone or HFD alone, which would help isolate the combined effect. Also, while L-Carnosine looks important, its potential to *prevent* osteoporosis wasn’t directly tested here, though other studies suggest it has anti-inflammatory benefits that could be relevant.
But this research opens up exciting possibilities for future work. Can we target the gut *microbiota* or specific metabolites like L-Carnosine to help prevent or treat osteoporosis in these situations? Could probiotics or dietary interventions that modify gut bacteria or boost beneficial metabolites be part of the solution? It gives us a new perspective, moving beyond just bone cells to look at the whole system – the “hypoxia-HFD-microbiota-bone” connection. It’s a complex puzzle, but studies like this are giving us the pieces to start putting it together.

Source: Springer