Decoding HCC Survival: The Power of Four Tiny RNAs
Hey there! Let’s dive into something super important in the world of health, specifically about a tough customer called Hepatocellular Carcinoma, or HCC. If you’re not familiar, it’s a major type of liver cancer, and honestly, it’s been a real challenge for doctors and patients alike. Predicting how someone with HCC might fare has always been tricky business. But guess what? Science keeps pushing forward, and I’ve been looking into some pretty cool findings about tiny molecules in our bodies that might hold some big answers.
The Unsung Heroes: Non-Coding RNAs
For the longest time, we thought a huge chunk of our DNA was just… well, junk. Didn’t seem to do much, didn’t code for proteins, the building blocks of life. But oh, how wrong we were! Turns out, these “non-coding RNAs” are actually incredibly busy little guys, playing all sorts of roles in how our cells work. Think of them as the conductors of a complex orchestra, making sure everything is happening when and where it should.
Among these non-coding RNAs, there’s a group called *long non-coding RNAs* (lncRNAs). And get this – they’re popping up as major players in diseases, including cancer. They can act like tiny switches, turning other genes on or off, influencing everything from cell growth to how cancer spreads. Pretty powerful for something we once ignored, right?
The Big Question: Can lncRNAs Predict HCC Survival?
So, knowing that lncRNAs are involved in cancer, a bunch of smart folks decided to ask a crucial question: Can we look at the *expression levels* (basically, how much of a specific lncRNA is present) in HCC patients and use that to predict their survival? This is a huge deal because having better predictive tools means doctors can make more informed decisions about treatment and care, giving patients the best possible shot.
The study I’ve been digging into aimed to do just that. They wanted to find new lncRNAs involved in HCC and see if their levels could predict patient outcomes. They used data from big public databases like The Cancer Genome Atlas (TCGA) and a couple of others (GSE135631 and GSE214846) – these are goldmines of genetic information from tons of patients.
How They Cracked the Code
Okay, so how do you go from a mountain of genetic data to a survival prediction model? It’s a bit like being a detective.
First, they looked at all the lncRNAs in the HCC samples compared to healthy liver tissue. They found a whole bunch that were either way *up* (overexpressed) or way *down* (downregulated) in the cancer samples. This is the first clue – if a molecule’s level changes significantly in disease, it’s probably involved somehow.
Next, they linked these lncRNA levels to patient survival data. Did high levels of a certain lncRNA mean a patient did worse? Or better? This step helped them narrow down the list to lncRNAs that seemed to have a prognostic impact.
Then came the crucial part: building a predictive model. They used fancy statistical methods (like Cox regression) to figure out which lncRNAs were *independently* associated with survival, meaning their predictive power wasn’t just due to other factors like the stage of the cancer or the patient’s age.

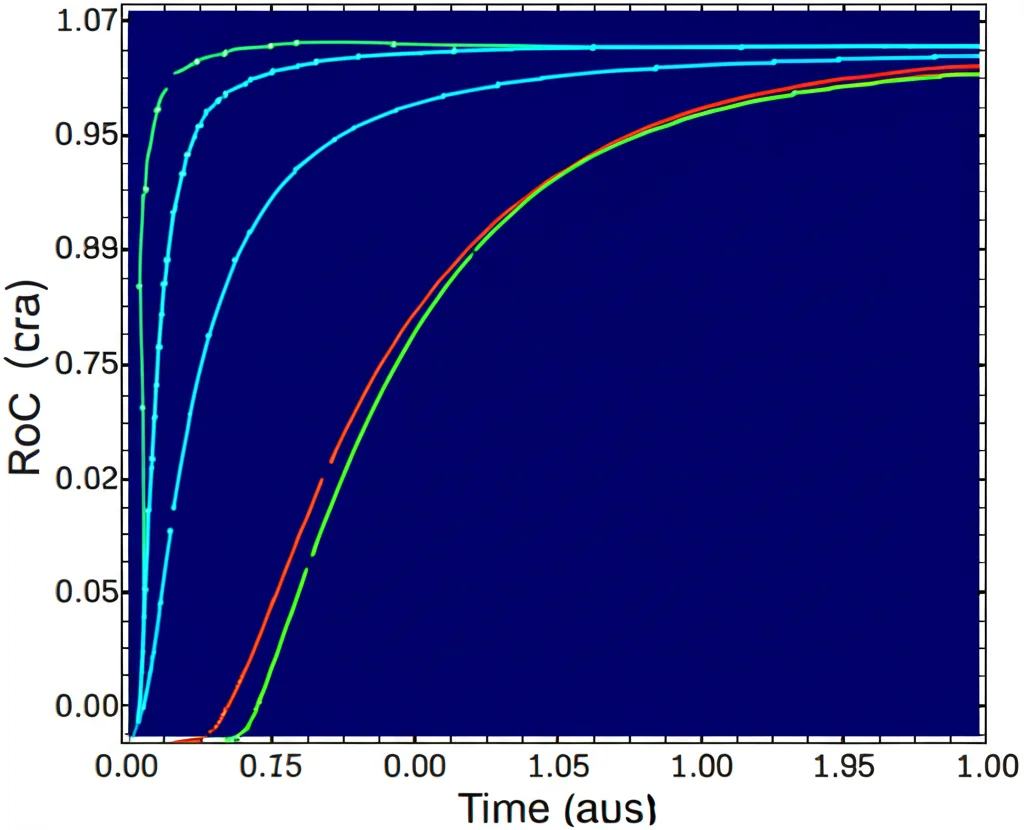
Finally, they built a “risk score” model based on the expression levels of these key lncRNAs. This score essentially tells you how high or low a patient’s risk of mortality is based on their lncRNA profile. They tested how well this model worked using different statistical tools (like Kaplan-Meier curves and ROC curves) and even validated some of their findings using actual tissue samples and a technique called RT-qPCR.
The Star Players Emerge
After all that detective work, a few lncRNAs really stood out. The study found that while many lncRNAs were dysregulated and linked to prognosis, four, in particular, seemed to be independent predictors of survival:
- AKR1B10P1
- RP11-465B22.3
- WASH8P
- NPM1P25
Here’s the interesting part: *overexpression* (higher levels) of AKR1B10P1, RP11-465B22.3, and WASH8P were linked to a *poorer* prognosis. Think of these three as potential trouble-makers, possibly acting like *oncogenes* (genes that promote cancer).
On the flip side, *downregulation* (lower levels) of NPM1P25 was linked to a *better* prognosis. This suggests that *higher* levels of NPM1P25 might actually be a good sign, potentially meaning it acts like a *tumor suppressor* (a gene that helps prevent cancer).
The multivariate analysis confirmed that these four were independent predictors, meaning their link to survival wasn’t just a coincidence tied to other clinical factors. That’s pretty powerful stuff!
The Predictive Model: A Glimpse into the Future?
Based on these four key lncRNAs, the researchers built their risk score model. And guess what? It worked! The model was able to effectively separate patients into high-risk and low-risk groups. Patients in the high-risk group (based on the expression pattern of these four lncRNAs) had significantly lower survival rates compared to those in the low-risk group.
They even checked the model’s accuracy over time using ROC curves, and it showed a solid ability to predict survival at the 5-year mark. The calibration was good too, meaning the predicted survival probabilities matched what was actually observed. This isn’t just a theoretical exercise; it’s a model that shows real promise for clinical use.
Validating these findings is crucial. The study used data from other independent datasets (GSE135631 and GSE214846) and found similar expression patterns for these four lncRNAs. They also specifically validated WASH8P expression in their own set of HCC tissue samples using RT-qPCR, confirming its significant upregulation in cancer compared to healthy tissue. Seeing the same results across different datasets and methods really strengthens the findings.
What Are These LncRNAs Actually Doing?
Finding out *which* lncRNAs are important is one thing, but understanding *how* they work is the next big step. The study looked at genes that were co-expressed (meaning their levels went up or down together) with these four lncRNAs. This gives clues about the biological pathways they might be involved in.
The three lncRNAs associated with poor prognosis (AKR1B10P1, RP11-465B22.3, and WASH8P) seemed linked to pathways heavily involved in cancer growth and progression, such as:
- mTORC1 signaling (involved in cell growth and metabolism)
- Glycolysis (how cancer cells get energy)
- Angiogenesis (forming new blood vessels to feed the tumor)
- Wnt-beta catenin pathway (involved in cell development and cancer)
- Reactive oxygen species (can cause DNA damage)
Pretty much all the usual suspects you’d find driving a tumor!

On the other hand, NPM1P25, the one linked to better prognosis, was associated with pathways related to:
- Fatty acid metabolism
- DNA repair
- Xenobiotic metabolism (dealing with foreign substances)
This is fascinating because issues with fatty acid metabolism are known to play a role in HCC development. Maybe NPM1P25 is involved in pathways that help keep things in check or repair damage, which would explain why higher levels are a good sign.
Why This Matters (And What’s Next)
So, what’s the takeaway from all this? Well, it looks like these four specific lncRNAs – AKR1B10P1, RP11-465B22.3, WASH8P, and NPM1P25 – aren’t just random molecules. Their expression levels are significantly and independently linked to how long HCC patients survive.
The risk model built using these four has a strong ability to predict patient mortality. This is incredibly exciting because it opens up possibilities for:
- Better *prognosis assessment*: Giving patients and doctors a clearer picture of what to expect.
- Potential *diagnostic biomarkers*: Maybe we can use these lncRNA levels to help detect HCC or understand its aggressiveness.
- Possible *therapeutic targets*: If these lncRNAs are driving cancer growth (like the first three seem to be), could we develop treatments to block them? Or could we boost the levels of protective ones like NPM1P25?
Of course, science is a journey. While these findings are super promising, the study mentions that they didn’t use fancy AI tools due to sample size limitations, which could potentially refine the model even further down the line. And while the *in silico* (computer-based) analysis and some validation are strong, more *in vitro* (lab cell studies) and *in vivo* (animal studies) work is needed to fully understand the exact molecular mechanisms at play.
But honestly, identifying these four lncRNAs and showing their power as independent prognostic markers is a massive step forward. It highlights just how much potential lies in understanding the “non-coding” parts of our genome.
It feels like we’re just scratching the surface of how lncRNAs influence cancer, but studies like this are paving the way for more precise, personalized approaches to tackling diseases like HCC. It’s a tough fight, but every new piece of the puzzle brings us closer to better outcomes for patients. Pretty hopeful, right?
Source: Springer