Cancer’s Sweet Spot: How Cells Hijack Metabolism and What PGAM2 Reveals
Hey there! Let’s talk about something super important in the fight against cancer, specifically hepatocellular carcinoma (HCC), which is a tough one, accounting for about 90% of liver cancer cases. Despite loads of brilliant minds working on it, we’re still figuring out all the sneaky ways these cancer cells grow and spread. That’s why digging deep into the molecular nitty-gritty is so crucial.
The Unexpected Player: PGAM2
So, there’s this enzyme called Phosphoglycerate mutase 2, or PGAM2 for short. Normally, it’s a key player in glycolysis, that basic process our cells use to turn sugar into energy. You find a lot of it in muscles, helping them power up. For a long time, its role in cancer, especially HCC, was a bit of a mystery. Its cousin, PGAM1, is known to be a bad guy, helping tumors grow by boosting glycolysis. So, you might expect PGAM2 to do something similar, right?
Well, guess what? Our recent findings threw a bit of a curveball. Turns out, in HCC tissues, PGAM2 levels are actually *lower* than in healthy tissue. Not only that, but the *acetylation* level of PGAM2 (a kind of chemical tag on the protein) is also reduced. This immediately made us wonder: if PGAM2 is *down* in cancer, what’s it actually *doing*?
PGAM2: The Unsung Tumor Suppressor?
To figure this out, we did some experiments. We looked at different HCC cell lines and saw that some had more PGAM2 than others. When we boosted PGAM2 in cell lines where it was low, their growth slowed down. They didn’t form as many colonies (clumps of cells, a sign of aggressive growth). On the flip side, when we *reduced* PGAM2 in cell lines where it was higher, they grew *faster* and formed *more* colonies.
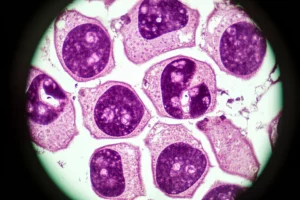
We didn’t stop there. We took these PGAM2-reduced cells and injected them into mice to see what would happen in a living system. And yup, you guessed it – the tumors that grew from these cells were significantly bigger and heavier than those from control cells. This was a big clue! It strongly suggested that PGAM2 isn’t a cancer promoter like PGAM1; it’s actually acting like a *tumor suppressor*, trying to keep things in check. Its downregulation in HCC is bad news because it removes a brake on cancer growth.
The Deacetylation Drama: SIRT2 Takes the Stage
Okay, so PGAM2 is a tumor suppressor and it’s downregulated in HCC. But *why* is it downregulated? We knew its acetylation level was lower, and acetylation is a crucial way cells regulate proteins – affecting everything from how stable they are to who they interact with. We honed in on a specific spot on PGAM2, a lysine residue at position 100 (we call it K100). Our previous work hinted that this spot’s acetylation was significantly reduced in HCC.
We suspected that removing the acetyl tag at K100 might be the key. Proteins called deacetylases do this job. One suspect was SIRT2, a member of the sirtuin family, which has been linked to PGAM2 deacetylation before. We found that SIRT2 *does* interact with PGAM2 in cells. When we inhibited sirtuins, the acetylation level of PGAM2 went up.
To confirm K100 was the main target, we created a version of PGAM2 that *mimics* the deacetylated state at K100 (we called it PGAM2-K100R). Compared to the normal PGAM2 (PGAM2-WT), this K100R version had much lower acetylation levels, even when SIRT2 was around. This told us SIRT2 is indeed zeroing in on K100.
What happens when K100 is deacetylated? We found that the deacetylated (K100R) version of PGAM2 was less stable and didn’t stick around as long in the cell. Why? Because deacetylation at K100 seemed to make PGAM2 a target for ubiquitination – basically, tagging it for destruction by the cell’s cleanup crew (the proteasome). More ubiquitination means faster degradation. And just like with PGAM2 knockdown, cells expressing this unstable, deacetylated K100R version grew faster and formed more colonies.

Then we brought SIRT2 back into the picture. Overexpressing SIRT2 led to lower PGAM2 levels, while inhibiting SIRT2 increased PGAM2 levels. And critically, overexpressing SIRT2 *reversed* the growth-inhibiting effects of PGAM2, while inhibiting SIRT2 *counteracted* the growth-promoting effects of PGAM2 knockdown. This pretty much sealed the deal: SIRT2-mediated deacetylation of PGAM2 at K100 is a major way HCC cells get rid of this tumor suppressor, paving the way for their growth.
Metabolism Makeover: PGAM2’s Unexpected Role in Glycolysis
Now, remember PGAM2 is a glycolytic enzyme? Cancer cells are notorious for their altered metabolism, particularly something called aerobic glycolysis, or the “Warburg effect.” They gobble up glucose and pump out lactate, even when there’s plenty of oxygen. It’s like they prefer a fast, inefficient energy pathway to build stuff and multiply quickly.
Given PGAM2’s role in glycolysis, we wondered how its downregulation affected this process in HCC cells. And wow, did it have an effect! When we overexpressed PGAM2, glucose uptake and lactate production went down. When we knocked PGAM2 down, they shot up. The same thing happened with the deacetylated K100R version of PGAM2 and when we overexpressed SIRT2 – more glycolysis. Inhibiting SIRT2, on the other hand, reduced the glycolysis boost caused by PGAM2 knockdown.
What’s fascinating is that PGAM2 usually works by converting one sugar molecule (3-PG) to another (2-PG). But the evidence suggests its role in suppressing aerobic glycolysis here might be *independent* of this specific enzymatic activity. It seems to be doing something else, perhaps through protein-protein interactions or influencing other pathways. We saw that when PGAM2 was low (either via knockdown or the K100R version), key enzymes involved in later steps of glycolysis, like LDHA, were upregulated. This pointed to LDHA as a potential downstream target.
The STAT3/LDHA Connection: Fueling the Fire
LDHA is a big deal in glycolysis; it’s the enzyme that makes lactate. Since LDHA levels went up when PGAM2 was low, we suspected PGAM2 might be suppressing HCC growth by keeping LDHA in check. We confirmed this: boosting LDHA reversed PGAM2’s inhibitory effects on glycolysis and cell growth, while blocking LDHA (either its expression or activity) counteracted the growth boost from PGAM2 knockdown. So, PGAM2 puts a damper on HCC growth by suppressing LDHA expression.
But how does PGAM2 influence LDHA levels? We dug into databases and found that a protein called STAT3 is known to bind to the promoter region of the *LDHA* gene, essentially telling the cell to make more LDHA. STAT3 is a well-known oncogene, often overly active in cancers. We found that when PGAM2 was low, STAT3 was more active and localized in the nucleus where it could turn on genes. Conversely, boosting PGAM2 reduced STAT3 activity.
Even more compellingly, inhibiting STAT3 activation not only reduced LDHA levels in PGAM2 knockdown cells but also wiped out their increased growth and colony formation abilities. This painted a clear picture: when PGAM2 is low (thanks to SIRT2), it somehow activates STAT3, which then ramps up LDHA production, fueling the aerobic glycolysis that cancer cells love, and driving HCC progression.

Fighting Back: Sorafenib and the SIRT2 Angle
Sorafenib is often the first-line treatment for advanced HCC, but resistance is a major problem. We wondered how PGAM2 levels affected the cells’ response to sorafenib. Surprisingly, knocking down PGAM2 actually made HCC cells *more sensitive* to sorafenib! They required a much lower dose to inhibit their growth. This was a bit counterintuitive, as lower PGAM2 promotes growth, but it suggests that perhaps PGAM2’s presence somehow contributes to resistance mechanisms, or its absence makes the cells vulnerable in a new way when hit with sorafenib.
Now, connect this back to SIRT2. We know SIRT2 downregulates PGAM2. We also found that SIRT2 levels are *higher* in sorafenib-resistant HCC cells compared to normal ones. And looking at patient data, high SIRT2 levels correlated with shorter survival times after sorafenib treatment. This strongly suggests SIRT2 plays a role in *acquired* resistance to sorafenib.
This seems a little contradictory, right? Lower PGAM2 (caused by SIRT2) makes cells *more* sensitive, but high SIRT2 is linked to *resistance*. The likely explanation is that while SIRT2 *initially* downregulates PGAM2, which might have a complex effect on sensitivity, SIRT2 also has *other* ways it promotes resistance (like affecting drug transporters or other pathways) that become dominant as cells develop resistance over time. The good news? Inhibiting SIRT2 (using a compound like AGK2) significantly reduced the viability of sorafenib-resistant cells, especially when combined with sorafenib. This points to a really exciting possibility: combining SIRT2 inhibitors with sorafenib could be a smart strategy to overcome resistance in patients.
Bringing It to the Clinic
To see if these findings held up in actual patients, we looked at HCC tissue samples. Just as our experiments suggested, PGAM2 protein levels were lower in tumor tissues compared to adjacent normal liver tissue. And confirming our SIRT2 findings, SIRT2 levels were higher in tumor tissues and showed a negative correlation with PGAM2 levels. Data from large databases also supported these trends and showed that high levels of both SIRT2 and LDHA correlated with more advanced tumor stages and poorer survival outcomes for patients.

This clinical data is super important because it backs up our lab findings and suggests that PGAM2, SIRT2, and LDHA aren’t just interesting molecules in a dish; they are relevant players in human HCC progression and could potentially serve as:
- Biomarkers: Measuring their levels might help predict how aggressive a tumor is or how a patient might respond to treatment.
- Therapeutic Targets: Developing drugs that boost PGAM2, inhibit SIRT2, or block LDHA (or STAT3) could offer new ways to fight HCC.
Putting It All Together
So, what’s the big takeaway? We’ve uncovered a pretty neat mechanism: In HCC, the enzyme SIRT2 gets busy deacetylating PGAM2 at a specific spot (K100). This deacetylation tags PGAM2 for destruction, lowering its levels. With less PGAM2 around, a signaling pathway involving STAT3 gets activated, which then boosts the production of LDHA. This surge in LDHA fuels aerobic glycolysis, giving cancer cells the energy and building blocks they need to grow and spread like wildfire. And to top it off, this whole SIRT2-PGAM2 axis seems tangled up in how HCC cells become resistant to standard treatments like sorafenib, offering a potential strategy to improve therapy by targeting SIRT2.
It’s a complex dance of molecules, but understanding these steps is absolutely vital. It gives us new ideas for how to diagnose HCC earlier, predict its behavior, and most excitingly, develop new therapies or improve existing ones. This research provides valuable insights into cancer metabolism and post-translational regulation, opening up promising avenues for future research and hopefully, better outcomes for patients fighting HCC.
Source: Springer