Fighting Brain Cancer: How a Citrus Compound and Chemo Team Up Against Glioblastoma
Let’s talk about glioblastoma for a moment. It’s a really tough type of brain tumor, actually the most malignant kind we know. Despite our best efforts with surgery, radiation, and a chemotherapy drug called temozolomide (TMZ), the prognosis is still pretty grim. It’s like this tumor has a knack for resisting treatment, often by hijacking cellular pathways that help it survive and grow.
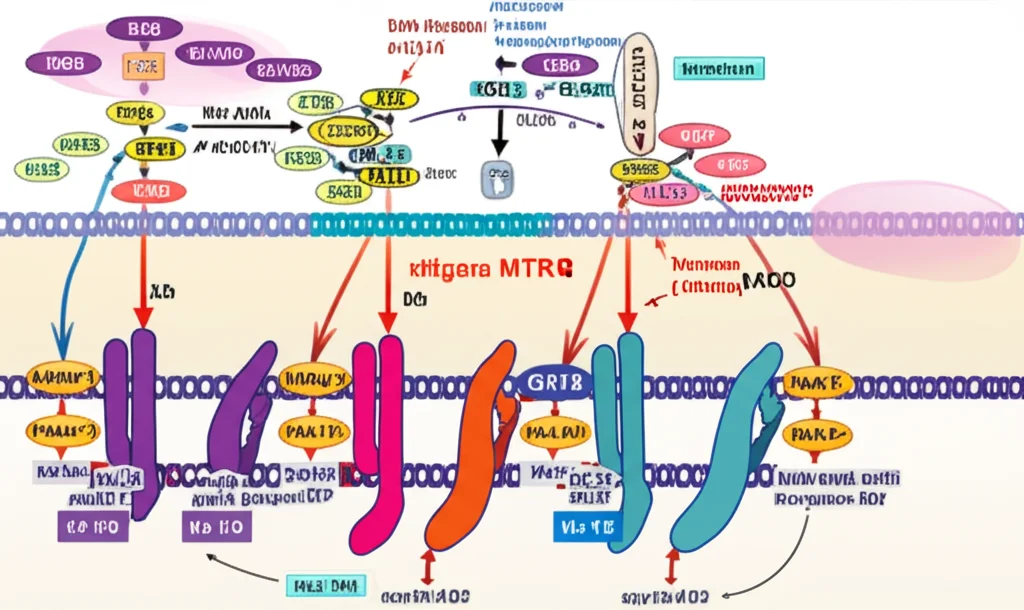
One of these key pathways is the PDK1/AKT/mTOR pathway. Think of it as a central command system for cell growth, survival, and even metabolism. In glioblastoma, this pathway often goes into overdrive, helping the tumor cells thrive when they really shouldn’t. So, naturally, researchers are keen on finding ways to shut it down or at least slow it down.
Now, enter hesperidin (HSP). This is a flavonoid, a natural compound found in citrus fruits. You might have heard about flavonoids having all sorts of health benefits – antioxidant, anti-inflammatory, and even anti-cancer properties. Hesperidin, in particular, has shown promise in lab studies, potentially triggering cancer cell death and preventing their spread. What’s really interesting is the idea that it might also help overcome chemoresistance.
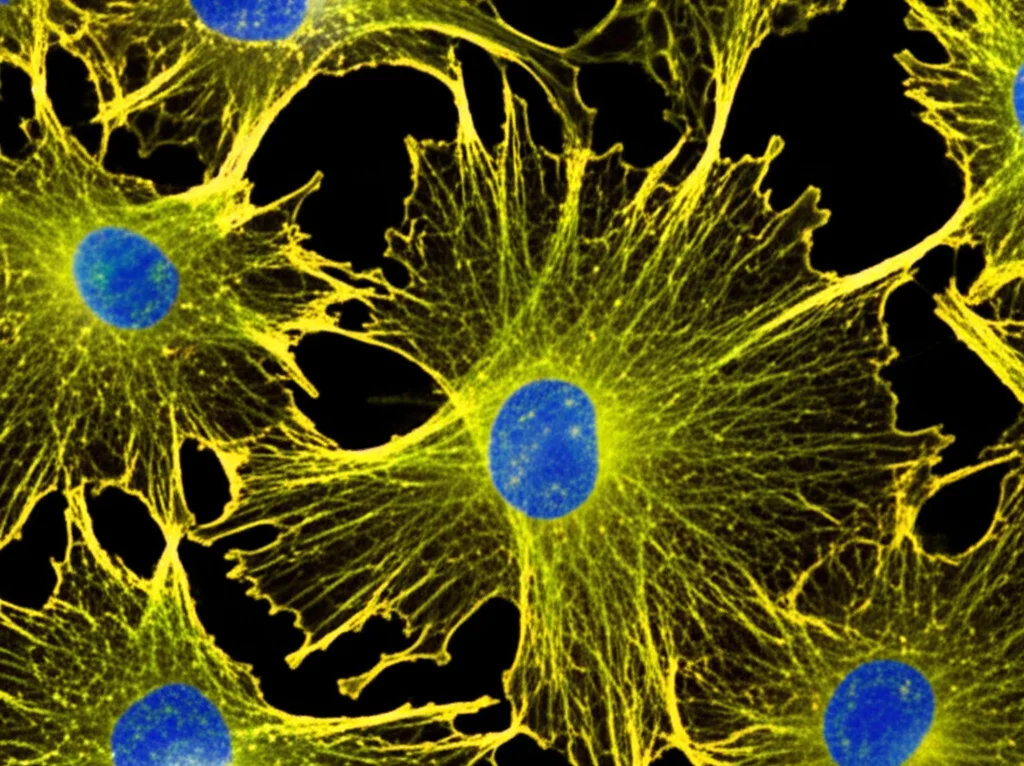
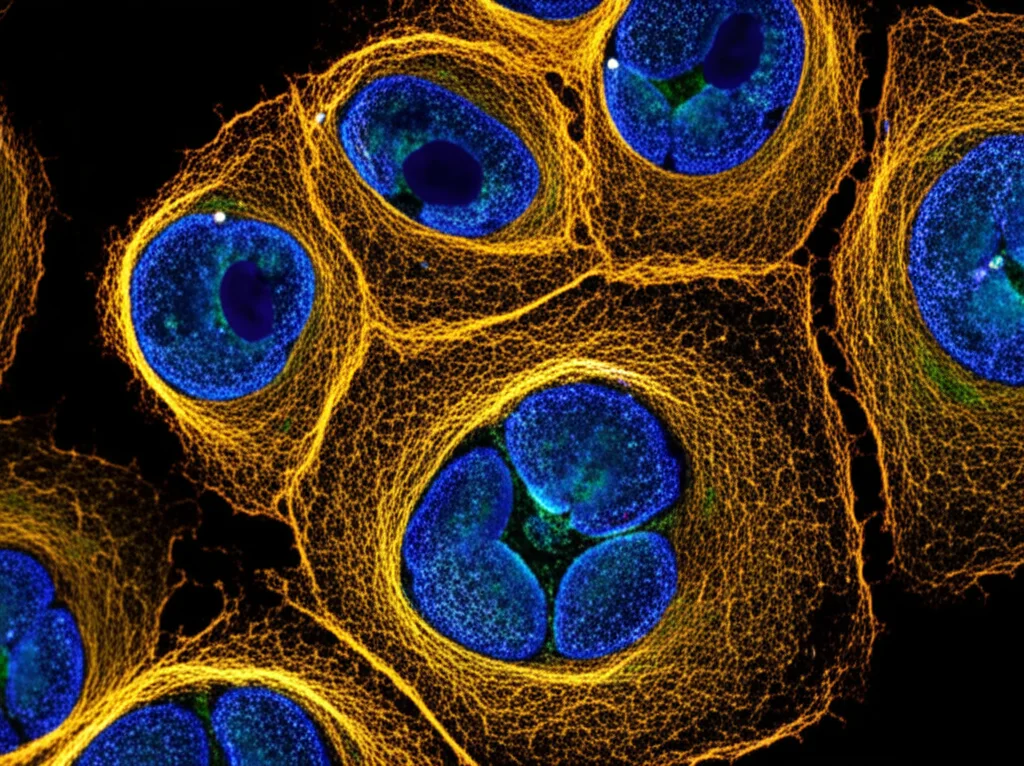
So, we thought, what if we bring these two together? What happens when you combine the standard chemo drug, TMZ, with hesperidin against glioblastoma cells? And not just what happens to the cells themselves, but also what happens to the tiny vesicles they release, called exosomes? Exosomes are like little packages cells send out, carrying messages in the form of proteins, mRNA, and microRNAs (miRNAs). These little messengers can influence other cells, including those in the tumor’s environment, and might even play a role in resistance and spread.
Our study aimed to dive into this exact question. We wanted to see how the combination of TMZ and different doses of hesperidin affected glioblastoma cells (specifically a line called T98G) and the exosomes they released, focusing on the PDK1/AKT/mTOR pathway and levels of certain miRNAs like miR-9.
Putting the Combo to the Test
We took our T98G glioblastoma cells and treated them with TMZ alone, different doses of hesperidin alone, and then the combination of TMZ with increasing doses of hesperidin (5, 10, 25, and 50 µg/mL). After 24 hours, we checked on them in various ways. We measured how many cells survived, how many were undergoing programmed cell death (apoptosis), levels of cell damage markers, oxidative stress, and importantly, the expression levels of key genes and miRNAs, both in the cells and in their isolated exosomes. We even looked at how hesperidin affected healthy cells (human dermal fibroblasts) to see if it was toxic to them.
The Results Are In!
What we found was pretty compelling. Hesperidin by itself did reduce the viability of the glioblastoma cells, but when we combined it with TMZ, the effect was significantly stronger. Especially at the higher dose of 50 µg/mL hesperidin alongside TMZ, cell viability dropped dramatically.
This reduced viability wasn’t just random cell death; it was largely due to increased apoptosis. We saw a significant rise in markers of apoptosis, like the activation of Caspase 3 and a shift in the balance of BAX and Bcl-2 proteins, which are key players in triggering cell self-destruction. The higher the hesperidin dose in the combo, the more apoptosis we observed.
Along with the cell death, we also saw signs of increased stress on the cells. Levels of LDH, a marker released when cells are damaged, went up. Oxidative stress markers increased, while the cells’ overall antioxidant capacity decreased. It seems the combination treatment was really putting the pressure on these glioblastoma cells.
Targeting the Master Switch: mTOR Pathway
Now, let’s get to the core pathway we were interested in. Remember the PDK1/AKT/mTOR pathway? In untreated glioblastoma cells, we saw that mTOR signaling was quite active, which makes sense for a fast-growing tumor. But with the TMZ-HSP combination, especially at higher doses, we observed a significant *decrease* in the levels of proteins associated with this pathway, specifically PDK1, AKT, and mTOR itself.
Conversely, we saw a significant *increase* in PTEN. PTEN is like the brakes for this pathway; it works to slow down the signaling. So, the combination treatment was not only hitting the accelerator (PDK1/AKT/mTOR) but also stepping on the brakes (PTEN). This dual action seems to be a powerful way to disrupt the tumor’s survival machinery.
Exosomes: Tiny Packages, Big Impact
Here’s where things get really interesting and, frankly, quite novel. We isolated exosomes from the treated glioblastoma cells. And guess what? The changes we saw in gene and miRNA expression in the cells were also reflected in the exosomes they released!
Specifically, we looked at miR-9 and miR-146-5p. These are small RNAs that can regulate gene expression. We found that the levels of both miR-9 and miR-146-5p were *upregulated* (increased) in the exosomes from the treated cells compared to the control. This is pretty significant because it suggests that the treatment isn’t just affecting the cells directly, but it’s also changing the messages they send out to their environment via exosomes. These altered exosomal messages could potentially influence surrounding cells or even distant sites, impacting things like metastasis or the immune response.
We also looked at the gene expression of components of the PDK1/AKT/mTOR pathway within the exosomes. Just like in the cells, we saw a decrease in PDK1 and AKT gene levels and an increase in PTEN gene levels in the exosomes from the treated groups. This is the first time, to our knowledge, that these changes have been shown at the exosomal level in glioblastoma cells treated with this combination.
Hesperidin’s Gentle Side: Protecting Healthy Cells
One crucial aspect of any potential cancer therapy is its effect on healthy cells. We tested hesperidin on human dermal fibroblasts, which are normal, healthy cells. We even created a “wound line” in a culture dish to see if hesperidin affected healing.
What we found was quite encouraging. Hesperidin, even at the highest dose we tested (50 µg/mL), did *not* show toxicity to these healthy cells. In fact, it seemed to have a protective effect! In the wound healing experiment, the hesperidin-treated groups showed increased cell viability and significantly faster wound closure compared to the untreated wound. It also helped reduce oxidative damage in these healthy cells. This suggests that while the TMZ-HSP combination is tough on glioblastoma cells, hesperidin itself might be gentle, or even beneficial, to normal tissues.
So, What’s the Takeaway?
Putting it all together, our study provides exciting initial evidence that combining temozolomide with hesperidin has significant anti-cancer effects on glioblastoma cells in the lab. It seems to work by:
- Significantly reducing cell viability and inducing apoptosis.
- Increasing cellular stress and oxidative damage.
- Crucially, inhibiting the pro-survival PDK1/AKT/mTOR pathway by decreasing PDK1, AKT, and mTOR levels and increasing the brake, PTEN.
- Changing the molecular cargo of exosomes released by the cells, including increasing levels of miRNAs like miR-9 and miR-146-5p, and altering pathway gene expression within these vesicles.
The fact that the changes are seen not just in the cells but also in their exosomes is particularly interesting. Exosomes play a role in how tumors communicate and spread, so altering their content could potentially impact metastasis.
What’s also promising is that hesperidin didn’t harm healthy cells in our tests; it actually seemed to protect them and promote healing. This suggests a potentially favorable side effect profile compared to therapies that are toxic to all dividing cells.
Looking Ahead
Of course, this is just a preliminary study in a lab setting using a specific cell line. There are limitations; for instance, we didn’t do a super detailed characterization of the exosome particles themselves (like size distribution analysis). And most importantly, these findings need to be validated in more complex systems, like animal models, before we can even think about human trials.
But our results provide a solid foundation for future research. They are the first to show the effects of the TMZ-HSP combination on both glioblastoma cells and their exosomes, particularly concerning the mTOR pathway and exosomal miRNA profiles. It really highlights the potential therapeutic value of this combination and opens up new avenues for understanding how it might work, including its impact on those tiny, powerful exosome messengers. We’re definitely planning to take this to the next level with animal studies!
Source: Springer