The GFI1 Blueprint: Keeping Our Immune Memory Sharp
So, you know how your body remembers past infections? Like that time you had the flu, and hopefully, your immune system learned a thing or two so the next encounter isn’t quite so rough? That’s your immune memory at work, and it’s absolutely essential for keeping us healthy, especially when we’re dealing with stubborn, long-term invaders like chronic viruses.
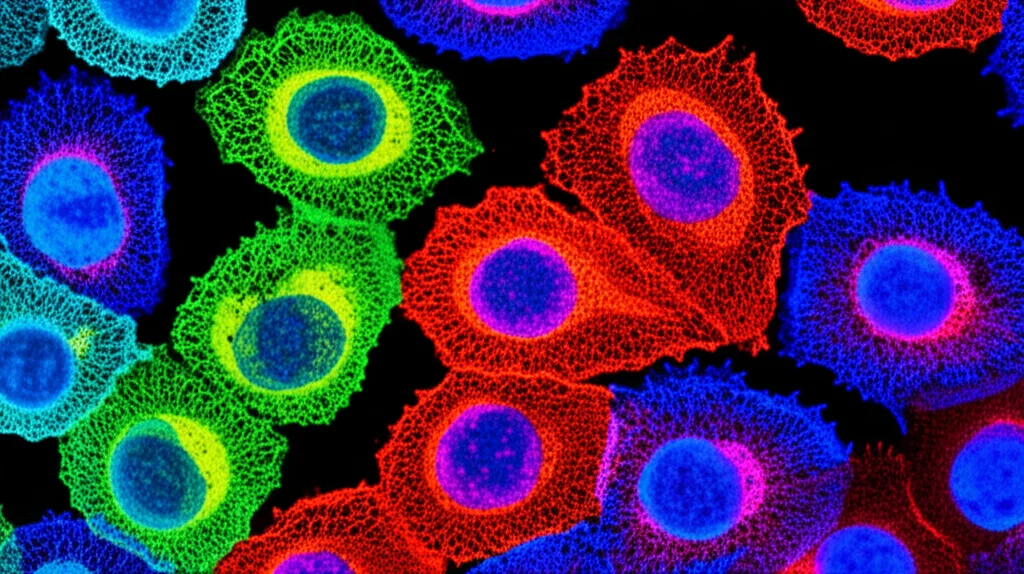
Our immune system has these amazing soldiers called CD8+ T cells. When they first meet a threat, they go through this incredible transformation. They multiply like crazy and turn into powerful “effector” cells that are really good at wiping out infected cells. But here’s the cool part: after the battle is won (or contained, in the case of chronic stuff), some of these soldiers don’t just disappear. They become “memory” cells. These memory cells are like the veterans of the immune army – they stick around for a long time, sometimes decades, ready to spring into action much faster and stronger if the same threat shows up again.
Now, within this memory crew, there are different types. You’ve got your central memory (TCM) cells and, even more special, stem cell memory (TSCM) cells. These TSCM cells are the real MVPs for long-term immunity because they can not only remember the threat but also renew themselves and produce *more* effector cells when needed. Think of them as the strategic reserve, the ones who can keep the fight going over the long haul. But keeping these crucial memory cells in top shape, especially during chronic infections where the threat never fully goes away, is a complex job, and we’re still figuring out all the details.
Meet GFI1: The Memory Cell’s Secret Keeper
This is where our story gets interesting. We’ve been looking closely at a protein called GFI1. It’s known as a transcriptional repressor, which basically means it helps control which genes in a cell are turned on or off. We wanted to see what GFI1 was up to in these CD8+ T cells, particularly during viral infections.
What we found was pretty neat. Using special ‘reporter’ mice where we could easily see GFI1 activity, we observed that GFI1 is highly expressed in those ‘naive’ CD8+ T cells (the ones who haven’t met a threat yet). When these cells get activated by an infection, GFI1 expression generally goes down. But here’s the key: it stays *high* specifically in the memory subsets, especially the TSCM and TCM cells. The effector cells, the ones doing the immediate heavy lifting, had much lower GFI1. This suggested GFI1 might be selectively important for those long-lived memory populations.
When GFI1 Goes Missing: Trouble for Memory
To really understand GFI1’s role, we created mice where we could specifically remove GFI1 from mature CD8+ T cells. We then infected these mice with viruses that cause chronic infections, like certain strains of lymphocytic choriomeningitis virus (LCMV) or murine cytomegalovirus (MCMV). What happened? Without GFI1, the antigen-specific CD8+ T cells (the ones trained to fight that specific virus) just didn’t stick around. Their numbers dwindled over time, especially the crucial TSCM and TCM populations.
It wasn’t just that they disappeared; they also showed reduced ability to multiply. This progressive loss of memory T cells meant the immune system failed to keep the chronic infection under control effectively. This told us loud and clear: GFI1 is absolutely critical for the long-term persistence of memory CD8+ T cells during chronic viral battles.
Peeking Inside: GFI1’s Molecular Blueprint
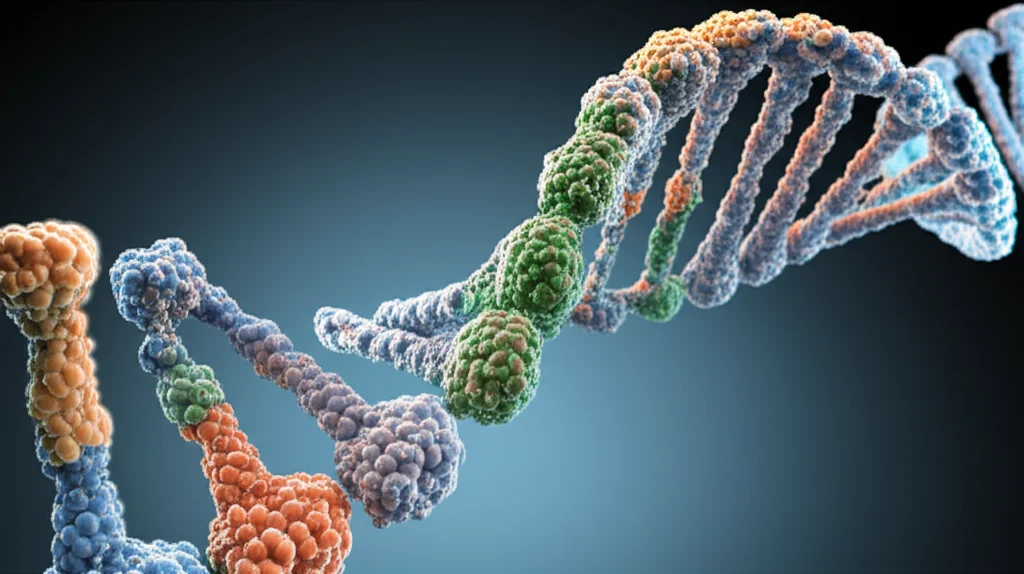
Okay, so GFI1 is essential for keeping memory cells around, but *how* does it do it? We dug into the cells’ genetic programs and even looked at how the DNA is packaged (epigenetics), because GFI1 is known to mess with chromatin structure to repress genes.
When we compared cells with and without GFI1, we saw big differences. GFI1-deficient memory cells had problems with genes related to cell proliferation and the cell cycle – the machinery needed for cells to divide and multiply. Genes like Cdk1 and E2f2, important for pushing cells through their division cycle, were downregulated. On the flip side, genes that promote cellular quiescence, like Btg1 and Btg2 (which basically tell cells to ‘chill out’ and stop dividing), were upregulated when GFI1 was missing. This fits perfectly with our observation that GFI1-deficient cells don’t proliferate well.
We also saw changes in genes that define memory cell identity, like EOMES and TCF1, which were lower in GFI1-deficient cells. GFI1 seems to maintain the expression of these key memory transcription factors while suppressing genes associated with effector functions or exhaustion.
Looking at the epigenetic landscape (how the DNA is folded and accessible), we found that GFI1 deficiency led to increased accessibility in certain regions of the DNA, particularly near genes that were abnormally expressed. This suggests GFI1 acts like a gatekeeper, keeping certain undesirable genes silenced in memory cells by influencing chromatin structure. Our analysis even predicted that GFI1 directly binds to regions near genes important for proliferation and memory, like E2f7 and Eomes, and those related to quiescence, like Btg1.
Survival of the Fittest: GFI1 and BCL-2
Persistence isn’t just about being able to divide; it’s also about not dying off prematurely. We looked at survival genes and found that GFI1-deficient memory cells had lower levels of BCL-2, a key protein that prevents cells from undergoing programmed cell death (apoptosis). They also showed signs of increased apoptosis. This suggests GFI1 helps memory cells survive.
Interestingly, another transcription factor, EOMES (which was downregulated in GFI1-deficient cells), is known to promote BCL-2 expression and T cell survival. When we artificially boosted EOMES levels in GFI1-deficient cells, it helped restore BCL-2 expression and partially rescued their persistence, though it didn’t fully fix their proliferation problems. This tells us GFI1 promotes survival partly through EOMES and BCL-2, but it has other ways of ensuring memory cell fitness, particularly related to keeping that proliferative engine running.
Putting it to the Test: Function Matters
So, if GFI1 is needed for memory cell numbers, proliferation, and survival, does that translate to better immune function? Absolutely. We tested the ability of GFI1-deficient memory cells to respond to a second encounter with the virus (a ‘recall response’). They were severely impaired compared to normal memory cells. We also transferred these cells into mice lacking other immune components to see if they could control a viral infection. Mice receiving GFI1-deficient cells had much higher virus levels and showed more severe signs of illness compared to those receiving normal cells.
This really hammered home that GFI1 isn’t just keeping cells alive and dividing for no reason; it’s maintaining a population of memory cells that are functionally ‘fit’ and ready to protect us when needed. And here’s a final crucial point: we found that continuous expression of GFI1 is necessary to maintain these persistent CD8+ T cell responses during chronic infection. It’s not a one-time job; GFI1 needs to be there for the long haul.
The Big Picture: GFI1 as a Master Regulator
What we’ve learned is that GFI1 acts as a master regulator for CD8+ T cell memory, especially the crucial stem cell memory population, during chronic infections. It does this through a combination of transcriptional and epigenetic control. It keeps the genes needed for self-renewal and proliferation turned on (or prevents them from being turned off) and helps silence genes that would push the cells towards quiescence or exhaustion. It also promotes survival, partly by ensuring sufficient levels of BCL-2, linked to EOMES.
This selective expression and critical function of GFI1 in TSCM cells explain why these cells are so good at persisting and replenishing the effector pool during ongoing threats. Without GFI1, this vital memory compartment collapses, leaving the host vulnerable.
These findings are pretty exciting because they shine a light on a key mechanism that maintains long-term immunity. Understanding how GFI1 works could potentially open up new avenues for boosting immune responses in chronic infections, improving the effectiveness of vaccines, or even enhancing cancer immunotherapies, which often rely on getting T cells to persist and fight tumors over time. It seems GFI1 is a vital piece of the puzzle in building and maintaining a robust, long-lasting immune memory.
Source: Springer







