Bone Breakthrough: Targeting FABP4 for Postmenopausal Osteoporosis
Hey there! Let’s chat about something pretty important, especially as we get a little older: our bones. You know, those amazing structures that keep us upright and moving? Sometimes, they can get a bit fragile, and for many women after menopause, that’s a real concern. We’re talking about Postmenopausal Osteoporosis, or PMOP. It’s a condition where bone mass dips, making fractures a much bigger risk. It’s a huge deal globally, and honestly, the treatments we have aren’t always perfect – they can have side effects and don’t work for everyone.
So, scientists are always on the hunt for new ways to understand and tackle this. And guess what? They’ve been looking at something called FABP4. Now, FABP4 sounds super technical, but think of it as a little protein helper that moves fatty acids around inside our cells. It’s known for playing a role in things like metabolism and inflammation. Recent studies hinted it might be connected to bone health, but its direct link to PMOP was a bit fuzzy. Until now!
Connecting the Dots: FABP4 and Bone Density
I found it fascinating that this study started by looking at people. Turns out, in women with PMOP, their blood levels of FABP4 were higher, and those higher levels seemed to go hand-in-hand with lower bone mineral density. Like, the more FABP4, the less dense the bone. That’s a pretty strong clue! They saw the same pattern in mice that had their ovaries removed (a common way to study PMOP in the lab because it mimics the estrogen drop). This clinical and animal data really got me thinking – FABP4 isn’t just hanging out; it seems to be actively involved in this bone loss business.

Bone Builders vs. Bone Breakers: Where Does FABP4 Fit?
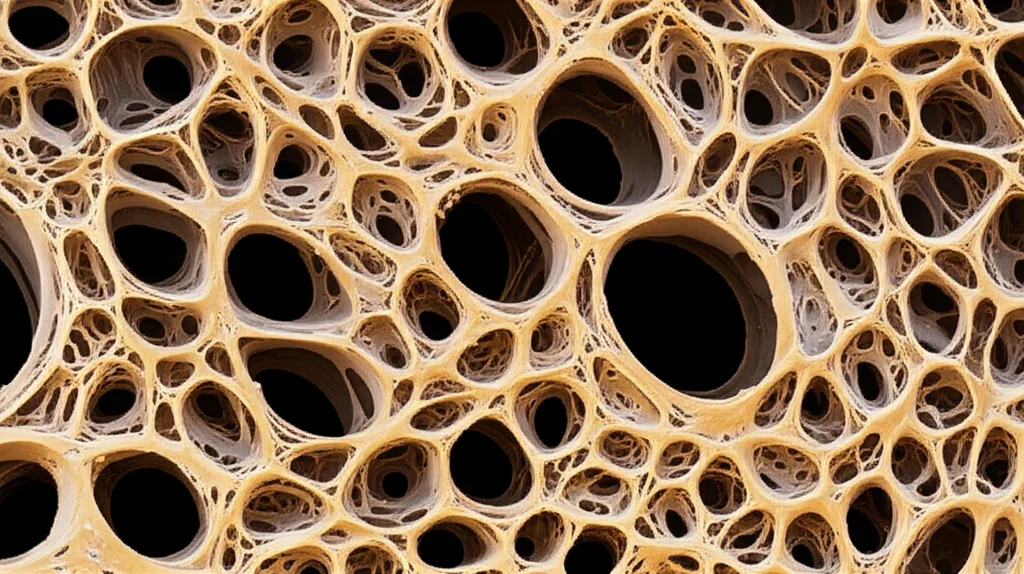
Okay, bone is constantly being remodeled. You’ve got cells that build new bone (osteoblasts) and cells that break down old bone (osteoclasts). In osteoporosis, the bone-breaking crew (osteoclasts) gets a bit too enthusiastic, and the bone-building crew (osteoblasts) can’t keep up. The big question was: Does FABP4 mess with the builders or boost the breakers? Or both?
The researchers did some clever experiments with bone cells in the lab. They added FABP4 to cells that *should* turn into bone builders, but… nothing really happened. FABP4 didn’t seem to stop the osteoblasts from doing their job. This was a bit surprising, but it pointed them in a clear direction.
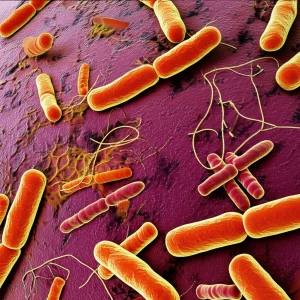
Then, they looked at the bone-breaking cells, the osteoclasts. And boom! Adding FABP4 significantly boosted the formation and activity of these osteoclasts. It made them better at breaking down bone tissue. This was a key finding – FABP4 seems to be cheering on the bone-breaking team, leading to that loss of density we see in PMOP.
Putting the Brakes on FABP4: The Inhibitor
If FABP4 is the problem, maybe blocking it is the answer? The study tested a specific FABP4 inhibitor called BMS309403 (let’s just call it BMS for short, way easier!). They found that BMS could stop those osteoclasts from forming. How? It turns out FABP4 influences a specific signaling pathway inside the cells – the Ca²⁺-Calcineurin-NFATc1 pathway. Think of it like a series of switches that need to be flipped for the osteoclasts to differentiate and get active. FABP4 seems to help flip those switches by increasing intracellular calcium, and BMS stops this process.
What’s really cool is that in lab tests, BMS was pretty potent at inhibiting osteoclasts, even comparable to alendronate, a common drug already used for osteoporosis. This got everyone excited about its potential as a new treatment.
Testing in Mice: Oral Delivery Challenges
Okay, lab tests are great, but the real test is in living animals. So, they gave BMS orally to the OVX mice. And yes, it did help! The mice treated with oral BMS had better bone mineral density and stronger bones compared to the untreated OVX mice. Success!
However, there was a catch. While it worked, the oral BMS wasn’t quite as effective as alendronate, even at a much higher dose. The researchers realized that FABP4 isn’t *just* in bone cells; it’s found in lots of tissues like fat, liver, heart, and muscles. Giving BMS orally means it goes everywhere in the body, and its effects might be diluted or complicated by inhibiting FABP4 in other places. Plus, the drug’s journey through the body (how it’s absorbed, distributed, and cleared) was affected by this widespread distribution. It wasn’t getting to the bone as efficiently as they hoped.
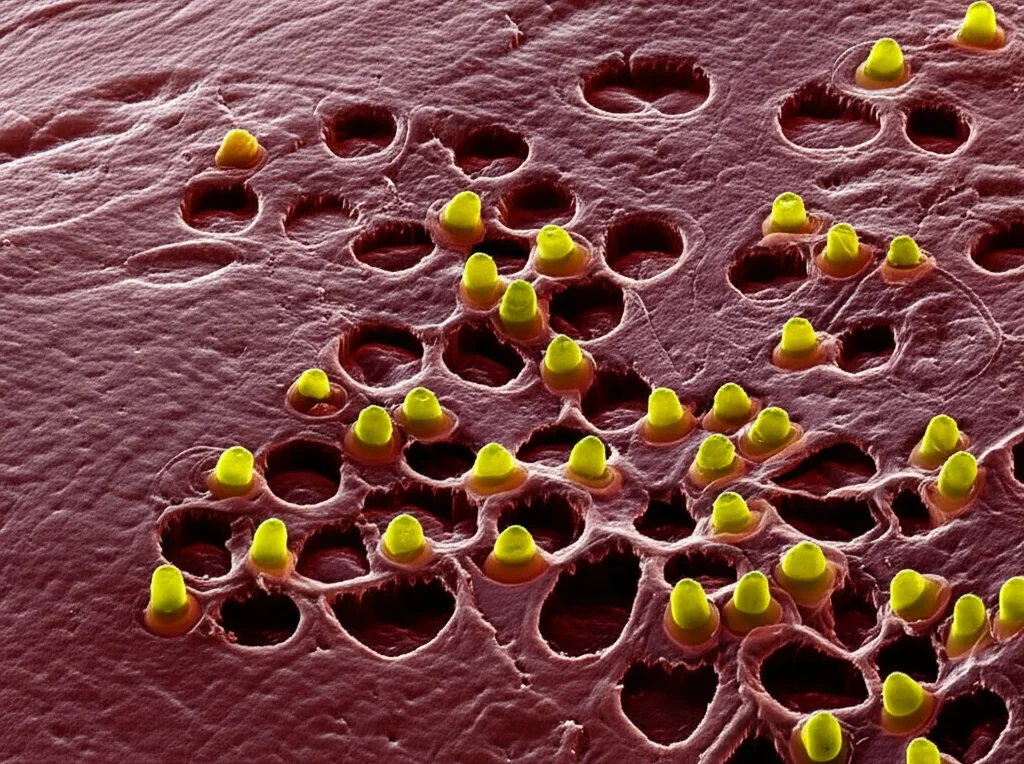
The Smart Solution: Bone-Targeted Nanoparticles
This is where the story gets really clever. If getting the drug to the bone is the challenge, why not *send* it directly there? The researchers designed tiny little carriers called nanoparticles. And here’s the ingenious part: they attached a bit of alendronate (remember that osteoporosis drug?) to the surface of these nanoparticles. Why alendronate? Because bisphosphonates like alendronate have a natural ability to stick strongly to bone tissue! It’s like adding a bone-seeking missile to the nanoparticle.
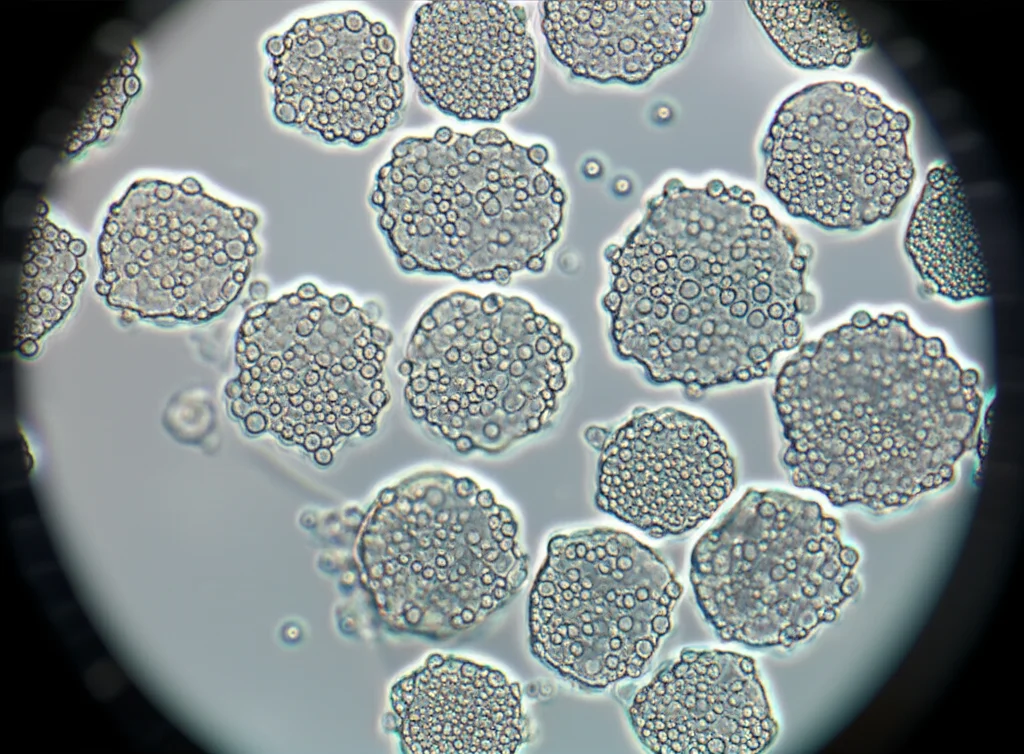
So, they loaded these bone-targeted nanoparticles (called Ald-BMS-NPs) with the FABP4 inhibitor, BMS. The idea is that when you inject these NPs, they’ll travel through the body, find the bone, stick to it, and then release the BMS right where it’s needed most – near the osteoclasts on the bone surface.
Direct Hit: Targeted Delivery Works!
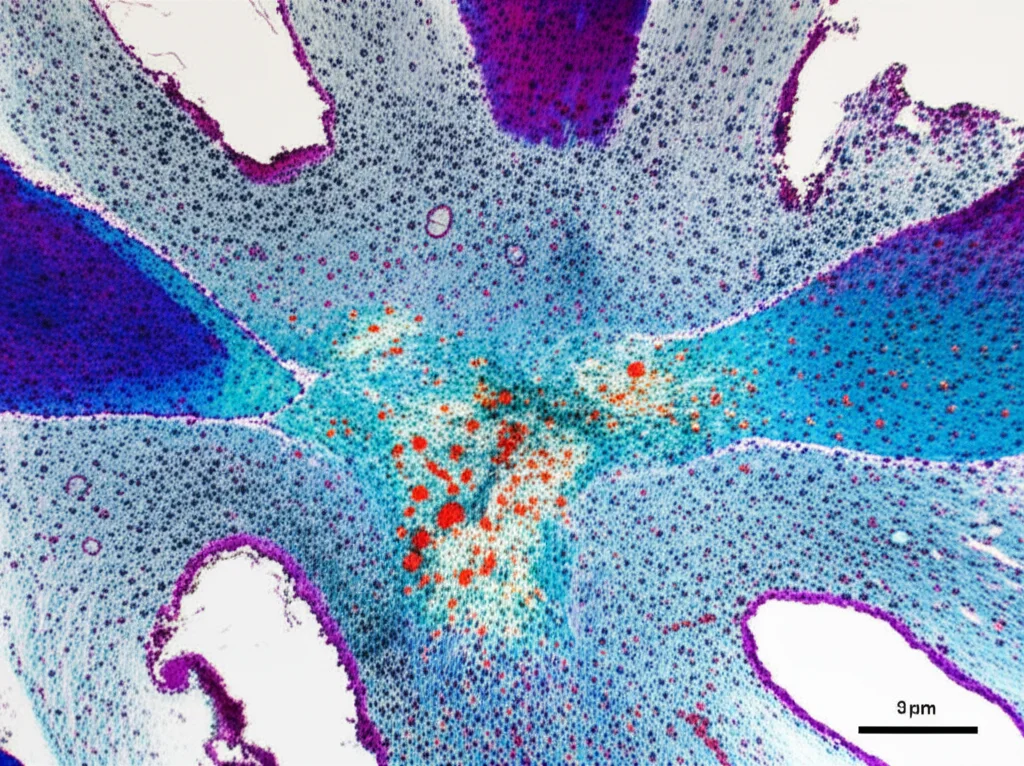
They tested these special nanoparticles in the OVX mice, giving them injections (intraperitoneal, into the belly, which is common for targeted therapies in mice). And wow, did it make a difference! The mice treated with the bone-targeted Ald-BMS-NPs showed significant improvements in bone density and structure. In fact, the efficacy was comparable to, and in some measures even slightly better than, the standard alendronate treatment. This confirms that getting the FABP4 inhibitor directly to the bone is a super effective strategy.
Plus, the nanoparticles seemed safe. They checked liver and kidney function markers and looked at tissue samples, and didn’t find any worrying signs of toxicity. This is crucial for any potential new therapy.
Why This Matters (Beyond Just Bone)
This research is exciting for a few reasons. First, it solidifies FABP4 as a key player in PMOP by specifically promoting bone breakdown. Second, it shows that inhibiting FABP4 is a viable therapeutic approach. And third, it highlights the power of targeted drug delivery. By using those clever bone-seeking nanoparticles, they overcame the limitations of systemic delivery and achieved fantastic results.
What’s even more intriguing is that FABP4 is linked to other metabolic conditions like diabetes and inflammation (which are also sometimes connected to bone problems). Targeting FABP4 could potentially offer a way to tackle multiple issues at once in some patients. It opens up possibilities for more personalized and effective treatments for osteoporosis and related diseases.
Looking Ahead
So, what’s the takeaway? This study gives us strong evidence that FABP4 is a critical factor in postmenopausal bone loss. Inhibiting it, especially when delivered directly to the bone using smart nanoparticles, looks like a really promising strategy. While clinical trials in humans are still needed, this research lays a solid foundation for developing new, potentially more effective, and safer treatments for PMOP. It’s a great step forward in the fight against fragile bones!
Source: Springer