When Your Nerves Muffle Your Eyes’ Cries: Diabetes, Neuropathy, and Dry Eye
Hey there! Let’s chat about something that affects a whole lot of folks, especially as we get a bit older or if we’re managing conditions like diabetes. We often hear about diabetes impacting our feet or kidneys, but did you know it can really mess with your eyes too, specifically that annoying thing called dry eye?
Now, dry eye itself is common, causing that scratchy, burning, or just plain uncomfortable feeling. But when you have Type 2 diabetes, things can get a little complicated. Sometimes, the very nerve damage that diabetes causes elsewhere in your body (what doctors call peripheral neuropathy) can also affect the nerves in your eyes. And here’s the kicker: these damaged eye nerves might make your eyes *less* sensitive. So, your eyes could be quite damaged and dry, but you might not feel the symptoms as strongly as someone without diabetes. It’s like the volume knob on your eye discomfort is turned down, making it tough to know how bad things really are. This can delay diagnosis and treatment, potentially leading to more serious issues down the road.
This is exactly the puzzle a group of clever researchers decided to tackle in the study we’re diving into today. They wanted to see if the symptoms of nerve damage *elsewhere* in the body could actually be a good indicator of how much damage was happening on the surface of the eye in people with Type 2 diabetes and dry eye.
What They Decided to Look At
So, how did they go about this? Well, they gathered a bunch of people. There were folks with Type 2 diabetes, and they split this group based on whether they showed symptoms of peripheral neuropathy using a specific questionnaire called the Michigan Neuropathy Screening Instrument Questionnaire (MNSIQ). Think of the MNSIQ as a checklist for nerve symptoms like tingling, numbness, or pain, mostly in the feet. They also included a group of people without diabetes to compare things to.
They then put everyone through a series of eye tests. They used the Ocular Surface Disease Index (OSDI) questionnaire to ask about dry eye *symptoms* (how scratchy or bothered their eyes felt). But they also did objective tests to look at the *signs* of dry eye and eye surface health. This included:
- Testing how sensitive the cornea (the clear front part of the eye) was.
- Checking for staining on the cornea, which shows damage to the surface cells.
- Measuring tear production.
- Looking at the quality and stability of the tear film.
- Assessing the meibomian glands (tiny glands in your eyelids that make the oily part of your tears – crucial for preventing evaporation).
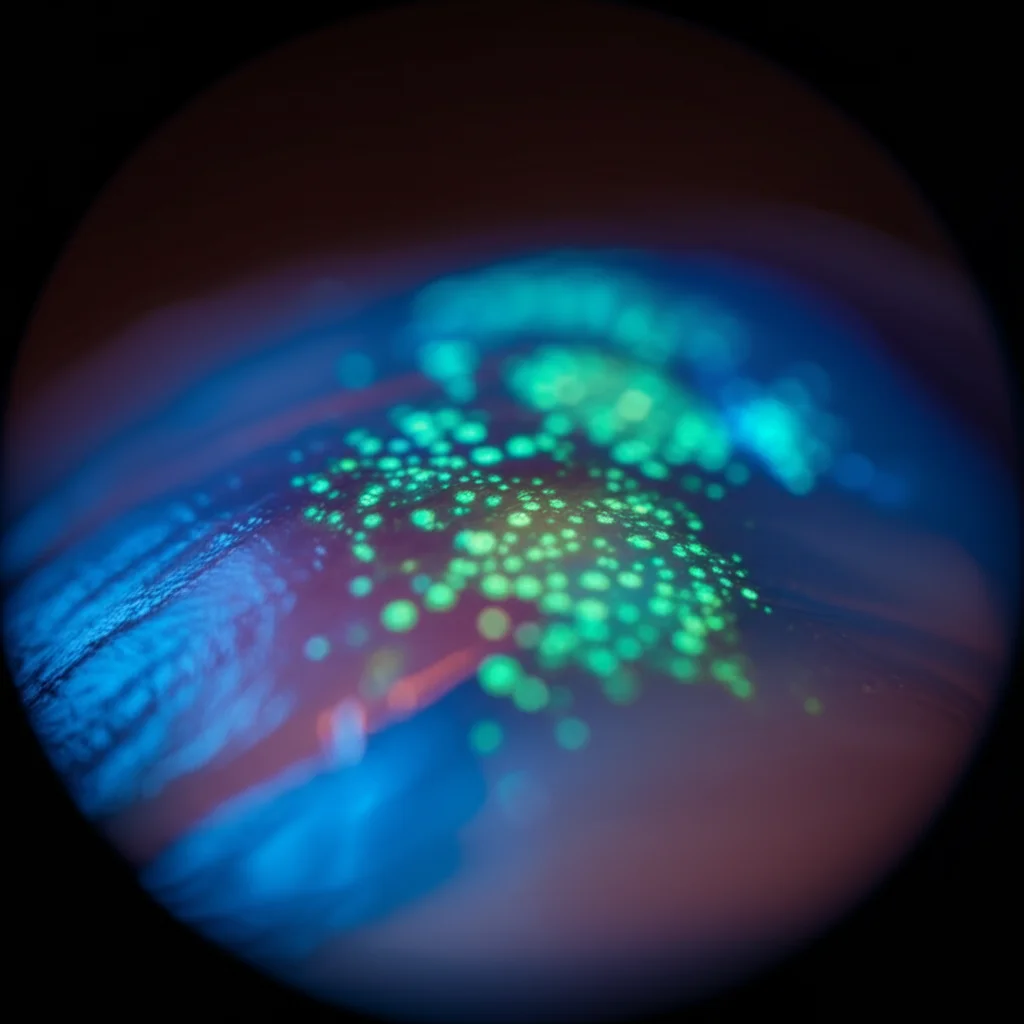
And here’s where the fancy tech came in: they used something called in vivo confocal microscopy (IVCM) to get incredibly detailed images of the tiny nerves right there in the cornea. They could measure things like how many nerves there were, how long they were, how branched they were, and even spot weird little bumps on the nerves called microneuromas.
The big idea was to see if the score on the MNSIQ (indicating nerve symptoms elsewhere) lined up with the results of these objective eye tests, especially the nerve imaging.

Okay, So What Did They Find?
This is where the study gets really interesting and confirms that initial puzzle.
First off, the dry eye *symptom* scores (OSDI) were pretty similar between the two groups of people with diabetes (those with MNSIQ-defined neuropathy and those without). This supports the idea that symptoms alone might not tell the whole story in diabetic patients. Both diabetic groups had higher OSDI scores than the non-diabetic controls, which isn’t surprising – dry eye is common with diabetes.
BUT, when they looked at the objective *signs*, a clear difference emerged. The group with MNSIQ-defined peripheral neuropathy had significantly *worse* objective findings compared to the diabetic group without neuropathy symptoms:
- More Corneal Staining: More damage visible on the eye surface.
- Worse Meibomian Gland Dysfunction (MGD): The oil glands weren’t looking good.
- Reduced Corneal Sensitivity: The eye surface was less able to feel touch.
- Significant Corneal Nerve Damage: The IVCM images showed fewer, shorter, and less branched nerves in the cornea, especially in certain areas.
- More Microneuromas: Those weird nerve bumps were much more prevalent and larger in this group.
And here’s the really important part: the MNSIQ score itself was strongly correlated with these objective eye signs! The higher the MNSIQ score (meaning more peripheral nerve symptoms), the worse the corneal staining, the worse the meibomian gland loss, and the more severe the corneal nerve fiber loss and microneuromas.
Interestingly, the MNSIQ score *didn’t* correlate significantly with the OSDI symptom score, tear production (SIT, TMH), or tear film stability (NIKf-BUT). This reinforces the main point: the MNSIQ is linking to the *physical damage* on the eye surface and the *nerve health* of the cornea, not necessarily how bothered the patient *feels* subjectively.
They also noted that people with MNSIQ-defined neuropathy tended to have had diabetes for longer and had higher HbA1c levels (a measure of long-term blood sugar control), which makes sense, as these are known risk factors for neuropathy and other diabetic complications.

Why This Matters for You and Your Eyes
So, what’s the big takeaway from all this? For me, it really highlights how interconnected our bodies are, especially with a systemic condition like diabetes. This study strongly suggests that if someone with Type 2 diabetes is starting to experience symptoms of nerve damage elsewhere in their body (like in their feet, picked up by the MNSIQ), it’s a serious red flag that their corneal nerves and ocular surface are likely also taking a hit, *even if* they aren’t complaining loudly about dry eye symptoms.
This is crucial because it means doctors shouldn’t rely *only* on how a diabetic patient says their eyes feel when assessing for dry eye and potential neurotrophic keratopathy (a more severe nerve-related corneal problem). The MNSIQ could be a simple, valuable tool to identify patients who need a closer look at their eye surface health, perhaps with more objective tests like staining or even that cool IVCM imaging if available.
The findings about the microneuromas are also super interesting. These little nerve bumps seem to be more common and more pronounced in diabetic patients with neuropathy, and they correlate with the severity of the neuropathy symptoms. They might turn out to be another objective sign doctors can look for to gauge the impact of diabetes on the corneal nerves.
Essentially, the study makes a strong case for including the MNSIQ in routine eye exams for people with diabetes. It’s a simple questionnaire that could potentially flag patients at higher risk for significant, yet possibly silent, ocular surface damage. Catching these issues earlier means doctors can intervene sooner and hopefully prevent more severe complications down the line.
A Few Things to Keep in Mind
Like any good research, this study has its limits. It was done with a specific group of patients in one location, and the sample size wasn’t huge. They also relied on the MNSIQ for peripheral neuropathy symptoms rather than more objective tests like nerve conduction studies, and they couldn’t account for *every* possible factor that might influence dry eye or nerve health (like smoking or sleep habits).
But even with these points, the core finding is pretty robust: the MNSIQ score is a good indicator of objective ocular surface and corneal nerve health in Type 2 diabetic patients, even when subjective symptoms don’t match up.
The Bottom Line
So, if you or someone you know has Type 2 diabetes, remember that keeping an eye on nerve health isn’t just about feet and hands. It’s about your eyes too! This study gives us a great reason to think about the MNSIQ as a potential screening tool in the eye doctor’s office. It could help uncover hidden problems and ensure that people get the right care for their dry eye and ocular surface, even when their symptoms aren’t screaming for attention. It’s all about connecting those dots and getting a clearer picture of what’s really going on.
Source: Springer







