Diabetes e Aortic Stenosis: A Tag Team Your Heart Doesn’t Want!
Hey there, heart-health enthusiasts! Ever wondered what happens when two tricky conditions like diabetes mellitus (DM) and aortic stenosis (AS) decide to team up in the body? Well, let me tell you, it’s not exactly a party for your heart. It’s more like they throw a wrench in the works, leading to a pretty distinctive set of challenges. We’ve been digging into this, trying to figure out exactly how DM messes with the left ventricle in folks who also have AS. We’re talking about inflammation, oxidative stress, and how these troublemakers impact the tiny powerhouses of the heart – the cardiomyocytes – and some super important signaling pathways.
So, What Did We Do?
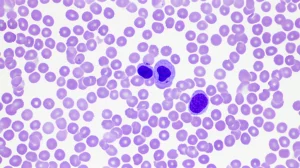
Alright, picture this: we got our hands on tiny pieces of heart muscle (left ventricular myocardial biopsies, to be precise) from 28 brave patients undergoing aortic valve replacement. Eleven of these patients had both AS and DM (our AS+DM group), and seventeen had AS but not DM (our AS-DM group). This way, we could compare what’s going on inside their hearts at a microscopic level. We were on the hunt for clues about inflammation, that nasty oxidative stress, how well the cardiomyocytes were functioning, the state of a giant protein called titin (super important for muscle elasticity!), and a crucial signaling pathway: the nitric oxide (NO)-soluble guanylyl cyclase (sGC)-cyclic guanosine monophosphate (cGMP)-protein kinase G (PKG) pathway. Sounds like a mouthful, I know, but it’s key to a happy heart!
Inflammation: The Fire Within
So, what did we find? Well, it turns out that in our AS patients who also had diabetes, the inflammation markers were through the roof! We used a cool technique called ELISA (Enzyme-linked immunosorbent assay, for the curious) and found significantly higher levels of pro-inflammatory baddies like high mobility group box protein 1 (HMGB1) and calprotectin. Think of these as little alarm bells that scream “inflammation here!”
And it wasn’t just the mediators; the receptors that these inflammatory signals dock onto were also more abundant. We saw more Toll-like receptor 2 (TLR2), TLR4, and the receptor for advanced glycation end products (RAGE). It’s like the heart cells in diabetic patients were more “receptive” to getting inflamed. This all correlated with an amped-up NOD-like receptor protein 3 (NLRP3) inflammasome – a major inflammation-driving complex – and a bigger release of interleukins (IL) 1, 6, and 18. These interleukins are like messengers that spread the inflammatory signal far and wide. Basically, the hearts of AS patients with diabetes were significantly more inflamed than those without diabetes. It’s a well-known fact that the build-up of AGEs (advanced glycation end products) is a big player in how AS gets worse, and our findings really highlight this. The downstream components of this inflammation cascade, like nuclear factor kappa B (NF-κB) and NLRP3, were also notably higher in the diabetic AS group. It’s a whole chain reaction of inflammation!
Oxidative Stress: The Rusting Effect
Now, inflammation often goes hand-in-hand with oxidative stress. Imagine it like rust forming inside the heart cells. In our diabetic AS group, we saw more signs of this “rusting.” Markers like hydrogen peroxide (H2O2) and the ratio of oxidative glutathione (GSSG) to reduced glutathione (GSH) were up in the heart muscle (myocardium) and even within the mitochondria – the cell’s energy factories. Interestingly, while 3-nitrotyrosine (another stress marker) and lipid peroxidation (LPO, damage to fats) showed some differences, the overall picture pointed to increased oxidative stress, especially in the mitochondria of diabetic AS patients. Mitochondria are a prime source of reactive oxygen species (ROS), those pesky molecules that cause oxidative stress. So, if they’re under duress, it’s bad news. This increased oxidative state isn’t just a bystander; it’s actively involved in making things worse.

The Stiff Heart Conundrum and a Key Pathway
So, we’ve got more inflammation and more oxidative stress. What does this do to the heart muscle itself? Well, it makes it stiffer. We measured something called passive stiffness (Fpassive) in individual cardiomyocytes. Think of it as how resistant the heart muscle cell is to being stretched. In diabetic AS patients, their cardiomyocytes were significantly stiffer, especially when stretched a bit more. This stiffness is a big deal because it can lead to problems with how the heart fills with blood, a hallmark of a condition called heart failure with preserved ejection fraction (HFpEF).
Why the stiffness? A lot of it boils down to that NO-sGC-cGMP-PKG signaling pathway I mentioned earlier. This pathway is crucial for keeping heart cells relaxed and elastic. In our diabetic AS patients, this pathway was seriously out of whack. We found:
- Impaired NO-sGC-cGMP-PKG signaling.
- Decreased phosphorylation (a type of chemical modification) of the giant protein titin.
Titin is like a molecular spring in the heart muscle, and its phosphorylation state directly affects how stiff or elastic it is. Less phosphorylation, especially at specific sites regulated by PKG, means a stiffer titin, and thus, stiffer cardiomyocytes. We saw that total titin phosphorylation was lower in the diabetic AS group, and specifically, PKG-dependent phosphorylation at a site called Ser4099 on titin was reduced. This is a direct hit to the heart’s ability to relax properly.
Can We Fix It? Hope from Treatments
Now for some good news! We didn’t just observe the problems; we also tried to see if we could reverse some of these changes, at least in the lab. We took those stiff cardiomyocytes from diabetic AS patients and treated them with a few things:
- Anti-inflammatory treatment: Using an IL-6 inhibitor (remember IL-6 was one of those inflammatory messengers?) actually helped normalize the elevated stiffness! It brought it down to levels comparable to the non-diabetic group. This tells us that inflammation is a major driver of that stiffness.
- Antioxidant treatment: We also used GSH (reduced glutathione), a natural antioxidant. Guess what? It also effectively normalized the cardiomyocyte stiffness in the diabetic AS group. So, tackling oxidative stress helps too! We even tried a mitochondria-targeted antioxidant called MitoTEMPO, which also reduced stiffness, though not quite to the non-diabetic levels, suggesting mitochondrial oxidative stress is a big part of the problem, but maybe not the whole story.
- Boosting the PKG pathway: When we directly applied PKG to the cardiomyocytes, it reduced stiffness in both groups, but the diabetic AS cells, while better, were still stiffer than the non-diabetic ones after treatment. This suggests the damage might be a bit more entrenched or that other factors are also at play.
- A Modern Diabetes Drug: We also tested empagliflozin (EMPA), which is a type of drug called an SGLT2 inhibitor, often used for diabetes. Excitingly, EMPA also reduced the stiffness in cardiomyocytes from diabetic AS patients! Again, not quite to non-diabetic levels, but a significant improvement. This is super interesting because SGLT2 inhibitors have been showing amazing heart benefits in larger studies.
Other Players in the Stiffness Game: PKA and CaMKII
It’s not just PKG that fiddles with titin’s phosphorylation. Two other protein kinases, PKA (protein kinase A) and CaMKII (Ca2+/calmodulin-dependent kinase II), also get involved. We found that PKA activity was reduced in the diabetic AS hearts, along with less PKA-dependent titin phosphorylation at another site (Ser4010). Treating these cells with PKA helped reduce stiffness, but again, the diabetic cells didn’t quite catch up to the non-diabetic ones.
Conversely, CaMKII activity and its expression were actually increased in the diabetic AS group. However, paradoxically, the CaMKII-dependent phosphorylation of titin at its specific site (Ser4062) was diminished. This is a bit of a head-scratcher and shows how complex these interactions are. Treating with CaMKII also reduced stiffness, with similar caveats as PKA and PKG. It seems like the whole system regulating titin is thrown off balance in diabetic AS hearts.

The Bigger Picture: A Link to HFpEF
So, why is all this molecular detective work important? Because these changes – the increased inflammation, oxidative stress, impaired signaling, and stiffer cardiomyocytes – are strikingly similar to what we see in heart failure with preserved ejection fraction (HFpEF). HFpEF is a type of heart failure where the heart muscle becomes stiff and can’t relax properly, even though its pumping strength (ejection fraction) might look normal. It’s a growing problem, and we’re still figuring out the best ways to treat it. Our findings suggest that when diabetes and aortic stenosis get together, they push the heart down a path that looks a lot like HFpEF. It seems HFpEF and AS might share common underlying mechanisms that get a nasty boost from diabetes.
This interplay is pretty complex. Diabetes doesn’t just make AS more common; it also makes it progress faster and hits the underlying damaging processes harder. Think heightened inflammation and oxidative stress fueling the calcification of the aortic valve – that’s diabetes adding fuel to the fire. Plus, things like high blood sugar, insulin resistance, and those pesky AGEs all trigger inflammation and mess with the blood vessel lining, making AS worse.
Our study really shines a light on how the heart muscle in patients with both DM and AS shows a full-blown inflammatory response. We’re talking higher levels of HMGB1 and calprotectin, more of their receptors (TLR2, TLR4, RAGE), and an overactive NLRP3 inflammasome churning out inflammatory interleukins. This isn’t just a local issue; it’s a systemic problem. For instance, it’s been shown that in diabetic patients, high HMGB1 is linked to more inflammation and vascular problems. And increased RAGE expression? That’s tied to endothelial dysfunction, a major problem in diabetes. It’s a vicious cycle where high blood sugar promotes AGEs, which activate RAGE, which worsens inflammation, which helps atherosclerosis and aortic calcification progress.
Oxidative Stress: A Double Whammy
The oxidative stress we saw isn’t just a side effect; it’s a key player. In diabetes, this stress (too many ROS, not enough antioxidants) can directly damage the aortic valve, making calcification and stenosis worse. But it also hits the heart muscle cells. ROS can mess with mitochondrial function, leading to energy problems and affecting how well the heart contracts. They can also directly modify important heart proteins, including those involved in calcium handling (crucial for contraction and relaxation) and signaling pathways like the kinases we talked about. All these roads lead to compromised cardiomyocyte function and that increased passive stiffness. There’s even a nasty feedback loop where ROS can speed up the formation of AGEs, and AGEs, in turn, can cause more ROS production. It’s a tough cycle to break.
This oxidative stress also directly attacks the bioavailability of nitric oxide (NO). NO is vital for activating that sGC-cGMP-PKG pathway. In diabetes, high blood sugar-induced oxidative stress means ROS gobble up NO, so there’s less available to do its job. This leads to less sGC activation, less cGMP, and ultimately, less PKG activity – a pathway critical for vasodilation, heart contractility, relaxation, and preventing bad remodeling. We’ve seen this pathway compromised in many heart diseases, including HFpEF and AS. Our study adds to the evidence that comorbidities like diabetes really worsen this impairment. Interestingly, while some studies point to “nitrosative stress” (too much NO-related modification) in HFpEF, our data didn’t confirm this as an additional problem on top of oxidative stress in our diabetic AS patients. Instead, we saw reduced NO production.

Titin: The Giant Spring Under Attack
Let’s talk a bit more about titin. This giant protein is a master regulator of diastolic function (how the heart relaxes and fills). Changes in which titin isoform is expressed (there’s a more compliant N2BA and a stiffer N2B) and its phosphorylation state are big deals in both DM and AS, especially when it comes to diastolic dysfunction and HFpEF.
Previous research on titin isoforms in AS has been a bit mixed, but our focus was on phosphorylation. The phosphorylation of titin’s springy bits by kinases like PKG, PKA, and CaMKIIδ can make titin less stiff, which is good. PKCα, on the other hand, can make it more stiff. Our findings of overall reduced titin phosphorylation, especially at those PKG and PKA sites in the diabetic AS patients, clearly link to that increased cardiomyocyte stiffness. Even when we tried to fix it by adding PKG or PKA back in the lab, the diabetic AS cells didn’t fully recover, suggesting the problem is pretty deep-seated, likely due to that intense oxidative and inflammatory environment. It’s not just titin, either. Fibrosis (scarring) and collagen deposition, which are worse in diabetes, also add to the heart’s stiffness.
What Does This Mean for Treatment?
Understanding these interconnected damaging mechanisms – the inflammation, oxidative stress, wonky titin, and stiff cells – is super important if we want to find better ways to help these patients. Our results showing that anti-inflammatory and antioxidant treatments could normalize cardiomyocyte stiffness, at least in the lab, are really encouraging. It suggests that targeting these pathways could be a game-changer.
And what about those SGLT2 inhibitors like empagliflozin? They’re already making waves in heart failure treatment. Our finding that EMPA reduced cardiomyocyte stiffness in diabetic AS patients is exciting because these drugs are known to reduce oxidative stress and inflammation and improve that crucial NO-sGC-cGMP-PKG signaling. They might offer a way to lessen the harmful effects of diabetes on the heart in AS patients. Of course, we need more research. Clinical trials have mostly looked at SGLT2 inhibitors in heart failure or diabetes without severe AS. We need to figure out if they’re safe and effective specifically for AS patients, with or without diabetes, especially since advanced AS can mess with hemodynamics in ways that might make some SGLT2i effects tricky. But the potential is there, especially with guidelines increasingly backing SGLT2is for various heart failure types.
Currently, for severe AS, fixing the valve (surgically or with TAVI) is the main treatment. But we don’t have meds that can stop or reverse AS progression. That’s why studies looking at drugs like DPP-4 inhibitors (another class of diabetes drugs) are also interesting, as some have shown promise in reducing heart stiffness in animal models by improving titin phosphorylation.
Wrapping It Up
So, to sum it all up, our deep dive into heart tissue shows pretty clearly that diabetes really throws a nasty curveball at patients who also have aortic stenosis. It cranks up inflammation and oxidative stress, messes with key signaling pathways important for cardiomyocyte health (like the NO-sGC-cGMP-PKG pathway), and ultimately leads to stiffer heart muscle cells. This whole scenario looks an awful lot like the early stages or features of HFpEF.
The silver lining? Our lab experiments suggest that tackling that inflammation and oxidative stress directly, or using smart drugs like SGLT2 inhibitors, could be promising avenues for treatment. It’s all about trying to protect those cardiomyocytes and keep the heart as healthy as possible, even when it’s facing this tough combination of conditions. More research is definitely needed to bring these ideas from the lab bench to the bedside, but it’s a hopeful step forward for a really high-risk group of patients!
Source: Springer