Vessel Guardians: Dapagliflozin Shields Against Injury in Young Men
Hey, Let’s Talk About Blood Vessels!
Alright, settle in, because I’ve got something pretty interesting to share from the world of medical research. You know how sometimes, after blood flow is cut off to a part of your body and then comes rushing back, it can actually cause *more* damage? It sounds weird, right? Like letting water back into a kinked hose should fix things, but sometimes the sudden rush causes new problems. This is called ischemia-reperfusion injury, or IRI for short, and it’s a big deal in things like heart attacks after doctors open up a blocked artery.
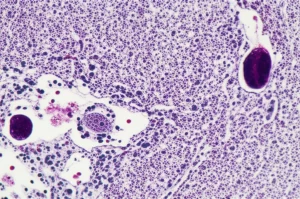
IRI can really mess with your blood vessels, specifically the inner lining called the endothelium. Think of the endothelium as the smooth, smart manager of your blood vessel traffic. When it gets damaged by IRI, it doesn’t do its job as well, like helping the vessel relax and open up when needed. Scientists have been hunting for ways to protect this crucial lining.
Enter dapagliflozin. You might have heard of it – it’s a drug mainly used for diabetes, heart failure, and kidney disease. But some earlier studies, mostly in animals, hinted that it might have protective effects on blood vessels, potentially shielding them from this IRI damage. So, the big question was: could it do the same in humans?
Putting Dapagliflozin to the Test
This is where the study I read comes in. It was a really well-designed trial – randomized, placebo-controlled, and double-blinded. That means participants were randomly assigned to get either dapagliflozin or a dummy pill (placebo), and neither they nor the researchers knew who was getting what. This is the gold standard for making sure the results are legit and not just due to chance or expectation.
They recruited 32 healthy young men, all around 27 years old. Why healthy young men? Probably to see the drug’s effect on vessels without the complications of existing diseases like diabetes or heart problems. The study focused on the forearm resistance vasculature – basically, the smaller blood vessels in the forearm. This is a common and reliable model for studying how blood vessels function in humans.
Here’s the cool part of the setup: they measured blood flow in the forearm before and after causing a temporary IRI. How did they do that? By inflating a cuff on the upper arm to a really high pressure for 20 minutes – enough to completely stop blood flow. Ouch! Then, they released the cuff, and blood flow rushed back in, creating that reperfusion scenario.
To see how the vessels were doing, they infused two different substances directly into the brachial artery (the main artery in the arm):
- Acetylcholine (ACh): This makes healthy endothelium release substances that cause the vessel to relax and blood flow to increase. It tests the endothelium-dependent function.
- Glyceryltrinitrate (GTN): This directly relaxes the smooth muscle in the vessel wall, bypassing the endothelium. It tests the endothelium-independent function – basically, the vessel’s ability to relax regardless of the endothelium.
They did these measurements *before* any treatment, then the guys went home and took either 10 mg of dapagliflozin or the placebo pill daily for 15 days. After those 15 days, they came back, took their pill for the day, and repeated the whole forearm ischemia and blood flow measurement process. The idea was to see if the 15 days of treatment changed how the vessels responded to the IRI.
The Big Reveal: Dapagliflozin to the Rescue!
So, what did they find? On the first day, before any treatment, the 20-minute forearm ischemia did exactly what IRI is known to do: it significantly reduced the endothelium-dependent vasodilation (the response to ACh) in *both* groups. The vessels were definitely impaired by the injury, which confirmed their model worked.
But here’s where it gets exciting! After 15 days of treatment, the picture changed dramatically. In the group taking the placebo, the IRI still caused that same dip in endothelium-dependent vasodilation. Their vessels were still getting damaged by the reperfusion.
However, in the group taking dapagliflozin, the IRI-induced impairment was *gone*! Their blood vessels responded to ACh just as well after the ischemia as they did before it. It was like the dapagliflozin treatment had built a shield around their endothelium, preventing the damage from happening.
Importantly, the response to GTN (the endothelium-independent test) wasn’t affected by IRI or the treatment in either group. This tells us that the basic ability of the vessels to relax wasn’t lost; the problem caused by IRI, and prevented by dapagliflozin, was specifically related to the endothelium’s function.
They also noted a small but significant drop in systolic blood pressure in the dapagliflozin group after 15 days compared to placebo, which is a known effect of the drug. And, as expected, most participants on dapagliflozin showed glucose in their urine, confirming the drug was working as it should (by making the kidneys excrete sugar).

Why This Matters and What’s Next
So, what’s the takeaway from all this? For the first time in humans, this study shows that a relatively short course of dapagliflozin can prevent the temporary damage to blood vessel function caused by ischemia-reperfusion injury in healthy individuals. This is a big deal because IRI contributes to problems in conditions like heart attacks and strokes.
How does it work? The study didn’t directly figure out the mechanism, but based on animal studies, scientists think dapagliflozin might:
- Activate pathways (like the AMPK-eNOS pathway) that help blood vessels produce more nitric oxide (NO), a key molecule for vessel relaxation and health.
- Reduce oxidative stress, which is like rust for your cells and is a major player in IRI damage.
This finding opens up some really exciting possibilities. Could giving dapagliflozin *before* procedures known to cause IRI, like certain heart interventions, help protect patients’ vessels and improve outcomes? It’s definitely a question worth exploring in future studies.
Now, let’s be realistic. This was a proof-of-concept study in healthy young men using a forearm model. Their blood vessels are likely much healthier than those in patients with heart disease, diabetes, or high blood pressure. The effects might be different, or even more pronounced, in people with existing vascular issues. Also, the forearm vessels might not behave exactly like the coronary arteries in your heart.
The researchers themselves point out that we still need to:
- Figure out the exact mechanism of how dapagliflozin provides this protection in humans.
- Test this in actual patients who are at risk of or experiencing IRI to see if it translates into real clinical benefits.
Despite these limitations, finding that dapagliflozin can prevent this type of vascular damage in healthy folks is a fantastic first step. It adds another layer to the growing understanding of this drug’s benefits beyond just managing blood sugar. It suggests new potential therapeutic avenues for protecting our precious blood vessels when they’re under stress.

So, while we wait for more research, it’s pretty cool to know that this drug, already helping people with other conditions, might also be a potential guardian for our blood vessels against injury.
Source: Springer