Gene Detectives: Pinpointing Cystinosis Culprits in the CTNS Gene
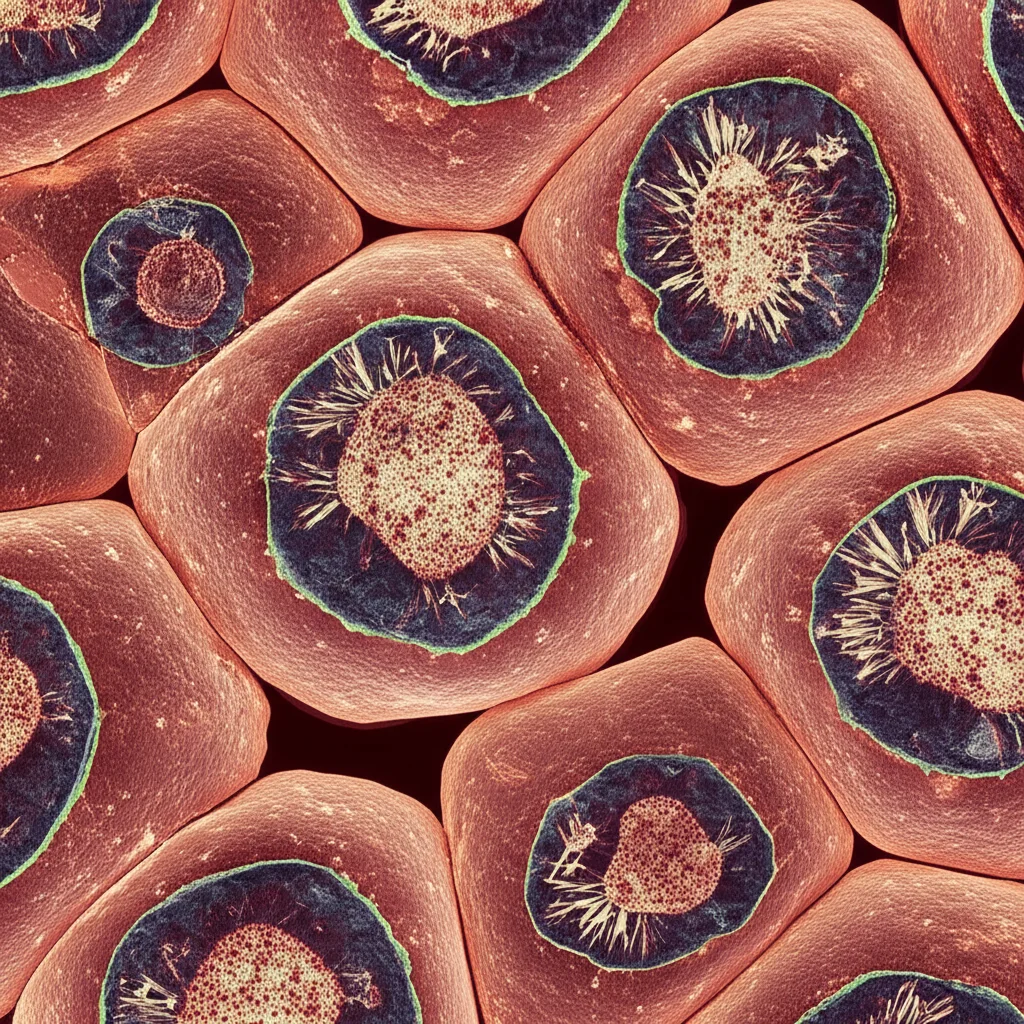
Hey there! Let’s chat about something pretty fascinating happening in the world of genetics and rare diseases. We’re diving into the nitty-gritty of a condition called Cystinosis. Now, this isn’t your everyday sniffle; it’s a rare genetic disorder that messes with how your body handles a specific amino acid called cystine. Think of it like a traffic jam inside your cells, specifically in tiny compartments called lysosomes, where cystine just piles up instead of being transported out properly.
This traffic jam is caused by faulty instructions found in a gene called CTNS. This gene is supposed to tell our cells how to make a protein called cystinosin, which acts like the exit ramp for cystine from those lysosomes. When the CTNS gene has mutations, the cystinosin protein doesn’t work right, or sometimes isn’t made at all. This leads to cystine crystals forming in various organs, causing damage, especially to the kidneys and eyes. It’s a tough condition, often showing up early in life.
Scientists have found over 140 different mutations in the CTNS gene. That’s a lot! But here’s the kicker: not all mutations are created equal. Some completely break the protein, while others might just slightly alter it. We’re particularly interested in something called nonsynonymous single nucleotide polymorphisms, or nsSNPs for short. These are tiny changes in the DNA sequence that result in a different amino acid being put into the protein chain. And changing even one amino acid can totally change how a protein folds, how stable it is, and ultimately, how well it does its job.
Why Go Digital? The Power of Computation
Traditionally, figuring out if a specific mutation is harmful involves a lot of lab work – growing cells, making the protein, testing its function. It’s crucial, but it can be slow and expensive. That’s where computational power comes in! Imagine being able to predict the effect of a mutation using powerful computer programs before even stepping into the lab. This is what in silico studies allow us to do.
This particular study, which I found absolutely intriguing, decided to play gene detective using these computational tools. Their mission? To find potentially harmful nsSNPs in the CTNS gene and predict exactly *how* they might mess up the cystinosin protein’s structure and function. They looked at a huge dataset – over 12,000 genetic variations – and zeroed in on the nsSNPs.
They didn’t just use one tool, oh no! They used a whole arsenal of predictive algorithms like SIFT, PolyPhen, CADD, MetaLR, and Mutation Assessor. Think of these as different expert opinions, each looking at the mutation from a slightly different angle (like evolutionary conservation, structural impact, etc.). If a mutation was flagged as potentially damaging by multiple tools, it was considered a strong candidate for being truly deleterious.
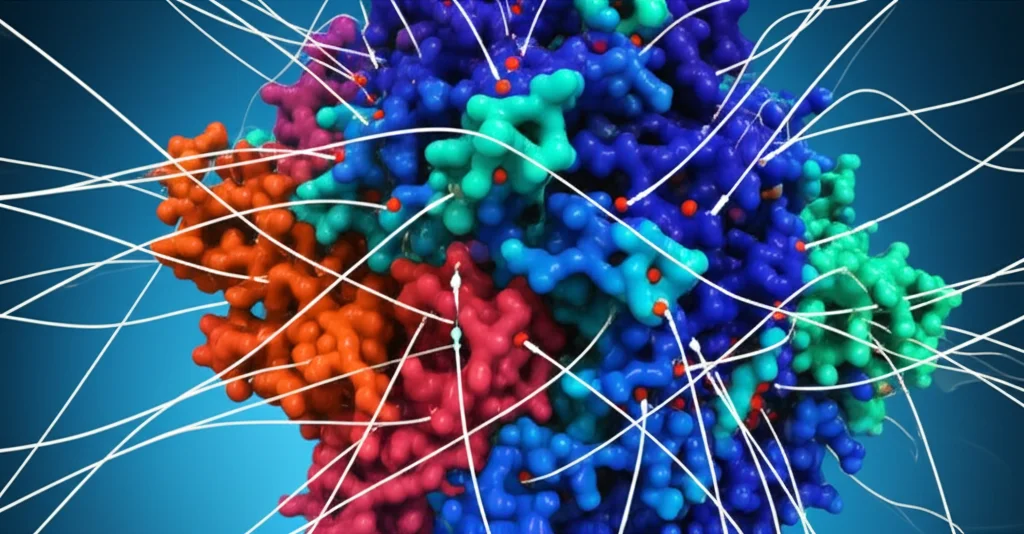
But they didn’t stop there. To get a really close look at how these mutations might physically affect the protein, they used something called molecular dynamics simulations. This is like creating a mini-movie of the protein in action, showing how it wiggles, folds, and interacts over time. By comparing the “wild-type” (normal) protein to the mutant versions in these simulations, they could see if the mutations made the protein unstable, too rigid, too floppy, or changed its shape in crucial areas.

Finding the Usual Suspects: Identifying Deleterious nsSNPs
Out of the initial 12,028 variations they looked at, 327 were nsSNPs – the kind that change an amino acid. Using their panel of predictive tools, they narrowed it down significantly. Only 19 of these nsSNPs were consistently flagged as potentially harmful by *all* the initial tools. That’s less than 6% of the nsSNPs, showing how powerful these filtering methods can be!
These 19 mutations were then put through even more tests using other tools like SNPseGO, PhD-SNP, PANTHER, and PROVEAN. And guess what? These tools largely agreed, predicting that most of these 19 variants were indeed likely to cause disease or disrupt protein function. It’s like getting confirmation from a second team of detectives.
The study specifically identified these 19 potentially deleterious nsSNPs:
- A137D
- S141F
- F142S
- R151G
- D161H
- S270F
- K280T
- K280R
- P283L
- Q284H
- S293G
- G296S
- S298G
- D305G
- G308R
- G308V
- G309V
- H353D
- Y357H
Some of these, like G308R and G308V, are already known to be pathogenic (disease-causing), which is great validation for the computational methods! Others, like A137D or D161H, were classified as having ‘uncertain significance’ in clinical databases, highlighting how this kind of computational study can help prioritize which variants need more experimental investigation.
Shaking Things Up: Impact on Protein Stability and Structure
Next, they looked at how these 19 mutations might affect the cystinosin protein’s stability. Using tools like I-Mutant 2.0, MUPro, and DynaMut2, they predicted whether the mutant proteins would be more or less stable than the normal version. The general consensus? Most of these mutations seem to make the protein *less* stable. Imagine building a house and swapping a load-bearing beam for a flimsy piece of wood – things are probably going to get shaky.
Specific mutations stood out as major destabilizers, particularly F142S and D305G. These were predicted to significantly reduce the protein’s structural integrity. On the flip side, a few mutations were predicted to be stabilizing or have minimal impact on overall stability, which is also important information!
The molecular dynamics simulations provided the visual evidence for these stability predictions. By tracking things like RMSD (how much the protein’s shape deviates over time), RMSF (how much individual parts wiggle), Rg (how compact the protein is), and SASA (how much surface is exposed to water), they could see the dynamic consequences of the mutations.
For example, the G308V mutation showed the highest RMSD, meaning it caused the biggest overall shape change compared to the normal protein. D305G and G308R led to increased local flexibility (higher RMSF), suggesting certain parts of the protein became floppy. G308V and G308R also increased the radius of gyration (higher Rg), indicating the protein became less compact. And F142S and G308R increased the solvent-accessible surface area (higher SASA), potentially exposing parts that should be tucked away inside.
These dynamic changes aren’t just theoretical wiggles; they directly impact function. The study highlighted how mutations like D305G and F142S, located in critical transmembrane domains (the parts of the protein embedded in the lysosomal membrane), could disrupt the protein’s ability to transport cystine. The G308 mutations, also in a transmembrane domain, were predicted to alter interactions crucial for transport.
Conservation and Connections: Why Location Matters
The researchers also looked at evolutionary conservation. Basically, how much has a specific amino acid position stayed the same across different species over millions of years? If a position is highly conserved, it usually means it’s super important for the protein to work correctly. They found that 16 out of the 19 potentially deleterious mutations were located at highly conserved positions. This strongly suggests that changing these specific amino acids is likely to have a big impact because nature has kept them the same for a reason!
They also explored protein interactions. Does cystinosin hang out with other proteins? Using tools like GeneMANIA and STRING, they predicted networks of proteins that might interact with CTNS. While these are computational predictions and need experimental validation, they suggested potential links to other transporter proteins and proteins involved in cellular metabolism and signaling. This hints that cystinosin might be part of a larger team working within the cell, and mutations could disrupt these team dynamics.
Spotlight on Specific Mutations
Let’s zoom in on a few of the key players identified:
- D305G: This one looks particularly nasty. It’s in a crucial transmembrane region and was predicted to cause major structural changes, including potentially losing a helix and altering how the protein interacts with metals. This residue is known to be vital for binding both cystine and protons, which is how cystinosin transports its cargo. Changing this aspartic acid (D) to a glycine (G) seems to severely disrupt this binding, leading to a complete loss of transport function according to previous studies.
- F142S: Located in another transmembrane domain, changing phenylalanine (F), a bulky hydrophobic amino acid, to serine (S), a smaller hydrophilic one, is like putting a square peg in a round hole in the membrane environment. The predictions showed this increases the protein’s exposure to water and destabilizes the cystine-binding area. Not good for a transporter that needs to sit snugly in a membrane!
- G296S: This mutation is in a cytoplasmic part of the protein. Glycine (G) is super flexible, and its presence often allows proteins to bend or move in specific ways. Swapping it for serine (S), which is bulkier and can form hydrogen bonds, can make that region more rigid. This loss of flexibility might mess with the protein’s ability to change shape during transport.
- G308R and G308V: Again, glycine (G) in a transmembrane domain (TM6). Changing it to arginine (R) or valine (V) introduces bulk and potentially charge (for arginine), disrupting the delicate balance needed for the helix to function correctly within the membrane. These mutations were predicted to significantly destabilize the protein and impact its transport capacity.
These detailed analyses help us understand *why* these specific mutations are likely harmful, linking the tiny change in DNA to the predicted disruption in protein function.
What Does This All Mean?
So, what’s the takeaway from this computational deep dive? Well, it gives us a much clearer picture of which specific mutations in the CTNS gene are most likely to cause problems in cystinosis. It highlights key amino acids and regions in the cystinosin protein (like G308, D305, F142) that are critical for its stability and ability to transport cystine.
These findings are super valuable because they provide a roadmap for future research. Instead of randomly testing mutations, scientists can prioritize these 19 candidates for experimental validation in the lab. Confirming their effects in real biological systems is the next crucial step.
Ultimately, understanding exactly how specific mutations break the cystinosin protein is essential for developing better treatments for cystinosis. If we know the precise structural and functional defects caused by different mutations, it might open doors for designing targeted therapies that could potentially fix or compensate for those specific problems. It’s a step forward in the fight against this challenging rare disease.
Source: Springer







