Unraveling COPD’s Grip: How a Key Inflammatory Player Hijacks Your Airways
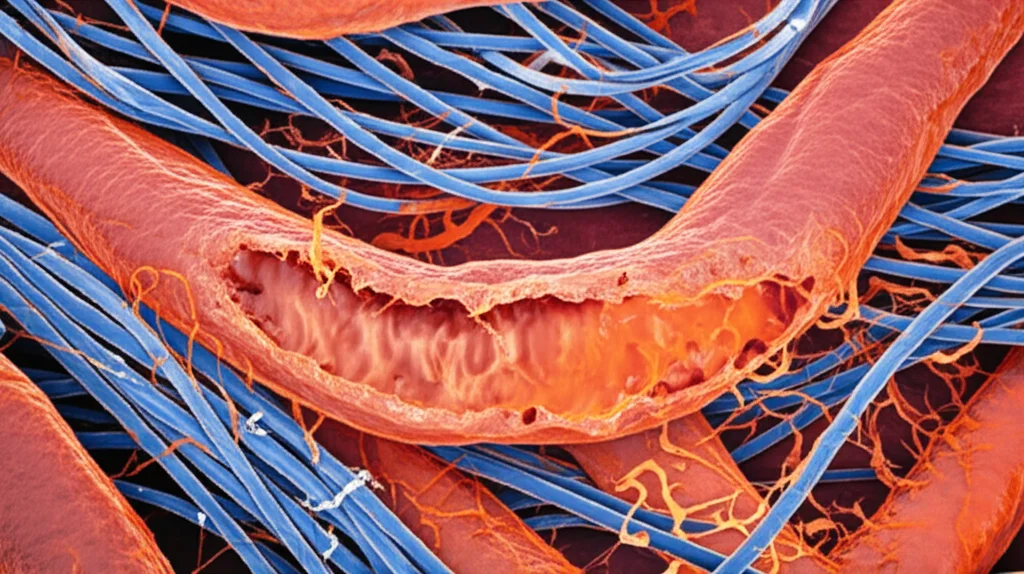
Hey there! Let’s chat about something pretty important – Chronic Obstructive Pulmonary Disease, or COPD. You know, that persistent lung condition that makes breathing a real struggle for so many folks worldwide. It’s a complex beast, and a big part of its nastiness comes down to something called airway remodelling. Think of it like the tubes in your lungs getting all messed up, thickened, and narrowed, making it hard for air to flow freely.
Scientists are constantly digging into *why* this happens, and it turns out inflammation is a huge culprit. One molecule that keeps popping up in the conversation is IL-17A. It’s a bit of an inflammatory troublemaker, and studies have hinted it’s involved in COPD, particularly with inflammation and laying down too much collagen – that stuff that makes tissues stiff.
But here’s where it gets really interesting. Our cells have this incredible internal recycling and cleanup system called autophagy. It’s essential for keeping everything running smoothly, getting rid of damaged bits, and maintaining balance. The big question researchers had was: could IL-17A be messing with this crucial cleanup process, and if so, how? And could that link back to the airway remodelling we see in COPD?
Setting the Scene: The COPD Challenge
So, as I mentioned, COPD is a major health headache globally. It’s not just one thing; it’s a mix of issues in the lungs and airways that lead to airflow getting stuck. We’re talking chronic inflammation, damage to the lining of the airways, and importantly, changes to the structure of the airway walls themselves. This remodelling involves things like the buildup of extra cellular matrix (ECM) – like collagen – and the muscles around the airways getting thicker. Smoking is a big driver, but genetics and other factors play a role too.
Enter IL-17A: The Inflammatory Player
Now, inflammation is key in COPD. There’s a specific type of immune cell, called Th17 cells, that produces a significant inflammatory factor: IL-17A. This molecule is like a signal flare, binding to its receptor (IL-17RA) on other cells. When it binds, it kicks off a whole cascade of events inside the cell, activating various signaling pathways. These activated pathways then tell the cell to release more inflammatory stuff, attracting other immune cells and generally fanning the flames of inflammation.
Studies have already connected high levels of IL-17A to fibrosis (scarring) in the small airways of people with COPD. And, interestingly, blocking IL-17A seems to help reduce both inflammation and fibrosis in airways. This tells us it’s definitely a player in the disease process.
Autophagy: The Cell’s Cleanup Crew
Let’s switch gears for a second and talk about autophagy. Imagine your cell is a busy city. Autophagy is like the waste management and recycling service. It collects damaged organelles, misfolded proteins, and other cellular debris, wraps them up, and sends them to the lysosomes (the cell’s recycling centers) for degradation. This process is vital for cell survival, renewal, and maintaining a healthy internal environment. In the context of airway remodelling, the breakdown of that extra ECM, like collagen, relies on this cleanup process. So, if autophagy isn’t working right, you can see how that extra stuff might build up, contributing to the thickening and stiffening of the airways.
The PI3K/AKT/mTOR Pathway: The Master Switch?
Okay, how does the cell decide *when* to do this cleanup? One major control center is a signaling pathway known as PI3K/AKT/mTOR. Think of it as a central hub that gets signals from growth factors, nutrients, and stress. When this pathway, particularly the mTOR part, is activated, it generally *inhibits* autophagy. It’s like the city manager deciding to cut back on the recycling services because resources are being directed elsewhere (like growth and building). Conversely, when this pathway is less active, autophagy gets a boost. This pathway has been implicated in lots of chronic inflammatory conditions and fibrosis, and studies have shown it can inhibit autophagy in lung fibroblasts.
Putting it Together: The Study’s Approach
So, we have COPD, IL-17A causing inflammation and fibrosis, autophagy needed for cleanup, and the PI3K/AKT/mTOR pathway potentially controlling autophagy. The big question is: does IL-17A use the PI3K/AKT/mTOR pathway to mess with autophagy in the cells responsible for airway remodelling, specifically bronchial fibroblasts?
To figure this out, the researchers did some pretty neat experiments. They created a mouse model that mimics the airway remodelling seen in COPD by injecting a virus carrying IL-1β (another inflammatory signal) directly into the airways. This method is good because it focuses the damage on the airways, similar to what happens in COPD, rather than causing widespread lung damage like emphysema (which smoking models often do). They also used an autophagy inhibitor (called 3MA) in some mice to see how blocking cleanup directly affected things.
They checked the mice’s lung function and looked at their lung tissue under the microscope using special stains (HE and Masson) to see inflammation and collagen buildup. They measured levels of IL-17A and other inflammatory markers (IL-6, CCL20). They also looked at autophagy directly using a super-powerful microscope (TEM) to count autophagosomes and measured key autophagy proteins (like P62, Beclin-1, and LC3) using a technique called Western Blot. Crucially, they measured the activity of the PI3K/AKT/mTOR pathway proteins (PI3K, AKT, mTOR) by looking at their phosphorylated (active) forms.

But that’s not all! To really pinpoint the role of IL-17A and its receptor on the key cells involved in remodelling – the bronchial fibroblasts (MBFs) – they isolated and cultured these cells from mice. They then used genetic tools (lentiviruses) to either make the cells produce *more* IL-17RA (overexpression or OE) or *less* IL-17RA (silencing or sh). They stimulated these modified fibroblasts with IL-17A and sometimes an autophagy activator (Rapamycin or Rapa) and then checked the activity of the PI3K/AKT/mTOR pathway and the levels of autophagy proteins. This *in vitro* (in the lab dish) part is super important because it lets them control the variables much more precisely than in the whole animal.
What They Found: The Key Results
The mouse model worked as expected – the mice showed signs of airway obstruction and the lung tissue looked like COPD, with thickened airways, inflammation, and increased collagen (both Collagen I and III).
In these COPD mice, they saw significantly higher levels of IL-17A, along with increased IL-6 and CCL20 (more inflammatory stuff!).
Now, for the autophagy part:
- In the COPD mice, the number of autophagosomes (those little cleanup bags) was significantly *reduced*.
- Key autophagy proteins showed that cleanup was inhibited: P62 (a protein that gets degraded during autophagy) was *increased*, while Beclin-1 and the active form of LC3 (LC3II/I ratio – markers of autophagy activity) were *decreased*.
- Immunofluorescence confirmed that LC3 levels were lower specifically in the bronchial fibroblasts within the mouse airways.
This all strongly suggests that autophagy is indeed suppressed in the airways during COPD remodelling.
Next, the pathway:
- In the COPD mice, the PI3K/AKT/mTOR pathway was clearly *activated*. The ratios of the phosphorylated (active) forms to the total proteins (p-PI3K/PI3K, p-AKT/AKT, and p-mTOR/mTOR) were all significantly increased.
This finding supports the idea that the activation of this pathway might be linked to the observed inhibition of autophagy.
The *in vitro* experiments using cultured bronchial fibroblasts (MBFs) provided even stronger evidence for the connection:
- When MBFs were engineered to *overexpress* the IL-17RA receptor and then stimulated with IL-17A, the PI3K/AKT/mTOR pathway was activated (increased phosphorylation ratios), and autophagy was inhibited (increased P62, decreased Beclin-1 and LC3II/I).
- Adding Rapamycin (which activates autophagy by inhibiting mTOR) reversed some of these effects, as expected.
- When MBFs were engineered to *silence* the IL-17RA receptor, stimulating them with IL-17A had a much weaker effect on activating the PI3K/AKT/mTOR pathway and inhibiting autophagy compared to cells with normal receptor levels.
These results from the cultured cells are pretty compelling. They show that IL-17A, specifically by binding to its receptor IL-17RA on bronchial fibroblasts, *does* activate the PI3K/AKT/mTOR pathway, and this activation *does* lead to the inhibition of autophagy in these key cells.
Now, there was a little wrinkle in the mouse study regarding the autophagy inhibitor 3MA affecting IL-17A levels, which made the *in vivo* pathway activation results a bit tricky to interpret definitively in that specific context. The researchers acknowledge this limitation, suggesting more studies are needed to fully clarify the complex interplay in the whole animal. But the strong *in vitro* data from the fibroblasts really supports the core hypothesis about the pathway and autophagy link driven by IL-17A.
Why This Matters
So, what’s the takeaway from all this detailed work? It seems we’ve uncovered a significant piece of the puzzle in how COPD airway remodelling happens. It’s not just inflammation floating around; it’s inflammation (specifically from IL-17A) actively interfering with the cell’s ability to clean and recycle itself via the PI3K/AKT/mTOR pathway. When this cleanup (autophagy) is inhibited in bronchial fibroblasts, these cells likely lay down more collagen and other ECM components without adequately degrading the old stuff, leading to the thickened, stiff airways characteristic of COPD.

This gives us exciting new targets for potential treatments! If we can find ways to:
- Block IL-17A signaling (maybe by targeting its receptor IL-17RA).
- Inhibit the activated PI3K/AKT/mTOR pathway in these specific cells.
- Or boost autophagy in bronchial fibroblasts.
…we might be able to slow down or even prevent the damaging airway remodelling in COPD. It’s a complex pathway, for sure, but understanding these molecular mechanisms is the first step toward developing more effective therapies for this challenging disease.
It’s a fascinating glimpse into the intricate cellular dance that goes wrong in COPD, and it highlights how crucial basic research like this is for paving the way to better health outcomes.
Source: Springer







