Beyond the Tumor Edge: AI and Ultrasound Predict Chemo Response in Breast Cancer
Hey there! Let’s chat about something pretty cool happening in the world of breast cancer treatment. We’re talking about predicting how well someone might respond to chemotherapy *before* they even start the whole course. Wouldn’t that be amazing? Knowing who’s likely to hit a home run (what doctors call a “pathological complete response” or pCR) means we can tailor treatments better, maybe dial back the tough stuff for some, or know others might need a different game plan from the get-go.
Right now, predicting this isn’t always easy. We’ve got biopsies, which are, you know, invasive. Genetic tests are super useful but can be pricey and not always standard practice everywhere. And sometimes, even a biopsy might miss the full picture because tumors can be a bit like a patchwork quilt – different bits responding differently. So, yeah, we’re really on the hunt for non-invasive, accurate ways to get this crystal ball view.
Why Predicting Response Matters
For folks with locally advanced breast cancer (LABC), neoadjuvant chemotherapy (NAC) – that’s chemo given *before* surgery – is a go-to move. The idea is to shrink the tumor, hopefully stop it from spreading, and maybe make surgery less extensive. And if you get a pCR? That’s fantastic news, often linked to better long-term outcomes. But here’s the kicker: not everyone responds. Some patients might go through all that tough treatment only for the tumor not to budge, or even worse, grow. And nobody wants to suffer through toxic side effects for little benefit. Finding a way to spot these non-responders early is a big deal.
Enter Radiomics and the ‘Neighborhood Watch’
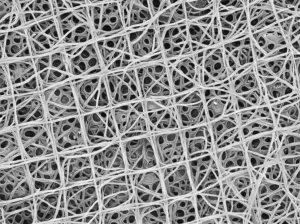
This is where things get really interesting. Imagine pulling tons of detailed data from regular medical images – stuff you can’t see with the naked eye. That’s radiomics! It’s like giving the image a super-powered magnifying glass and extracting patterns. Most studies using radiomics for cancer have focused on images like MRI, CT, or PET/CT. And often, they look *inside* the tumor itself. But what about the area *around* the tumor?
Think of the tumor as a house. What’s happening inside is important, sure, but the neighborhood – the surrounding tissue, the immune cells hanging around, the blood vessels – can tell you a lot about what’s going on and how the ‘house’ might react to visitors (like chemo). This ‘reactive zone’ around the tumor, the peritumoral region, hasn’t gotten as much attention in ultrasound studies, especially for predicting NAC response. Ultrasound is awesome because it’s convenient, affordable, and widely available. So, could looking at the *peritumoral* region using ultrasound radiomics (PURS) give us new clues?
This study I’m diving into decided to put this idea to the test. They wanted to see if PURS, combined with the power of machine learning, could predict pCR in LABC patients. And they didn’t just look at the ‘neighborhood’; they compared it to looking *inside* the tumor (intratumoral radiomics or IURS) and also to the standard stuff doctors already use (clinicopathologic factors like tumor type, hormone status, etc.).
Putting Machine Learning to Work
So, how did they do it? They gathered data from 358 patients with LABC who had ultrasound scans before starting NAC and then had surgery. They split the patients into a training group (to teach the machine learning models) and a test group (to see how well the models worked on new data).
Using some pretty sophisticated software, they extracted loads of radiomics features – over 850! – not just from *inside* the tumor (IURS) but also from a 3mm thick zone *around* it (PURS). It’s like getting a super detailed profile of both the house and its immediate surroundings from the ultrasound picture.
Then came the machine learning part. They tried out five different ML algorithms:
- Linear Discriminant Analysis (LDA)
- Support Vector Machine (SVM)
- Random Forest (RF)
- Logistic Regression (LR)
- Adaptive Boosting (AdaBoost)
These algorithms are like different types of detectives, each with their own way of finding patterns in the data to predict whether a patient would achieve pCR or not. They built separate predictive models using PURS, IURS, and the standard clinicopathologic factors.

The Big Reveal: What the Data Showed
Okay, drumroll please! What did they find? First off, in this group of patients, about 27% achieved a pCR. That’s roughly in line with what we see in other studies.
When they looked at the standard clinicopathologic factors (like hormone receptor status and HER2 status, which they found were indeed linked to pCR), the model based on these factors had a decent predictive ability, with an AUC (a measure of how well a model distinguishes between two groups) of about 0.76 in the test set. Not bad, but could we do better?
Now, for the radiomics models. They tested all five ML algorithms for both PURS and IURS. And guess what? The *Random Forest (RF)* classifier consistently came out on top for both!
* For the **PURS** models (looking at the neighborhood): The RF model had an impressive AUC of 0.889 in the test set. The other ML models were lower (LR 0.849, AdaBoost 0.823, SVM 0.746, LDA 0.732).
* For the **IURS** models (looking inside the tumor): The RF model was even better, hitting a maximum AUC of 0.931 in the test set. Again, RF outperformed the others (AdaBoost 0.920, LR 0.875, SVM 0.825, LDA 0.798).
So, comparing the three approaches:
- The RF-based **PURS** model (AUC 0.889) was significantly *better* than the clinicopathologic factors model (AUC 0.759). Yay, neighborhood data adds value!
- The RF-based **IURS** model (AUC 0.931) was significantly *better* than the PURS model. Okay, what’s happening inside the tumor still seems to be the strongest predictor here.
- And, naturally, the RF-based **IURS** model was also significantly *better* than the clinicopathologic factors model.
The RF classifier really shone, providing the highest accuracy and predictive power in both radiomics approaches. It seems like a really robust tool for this kind of prediction.
What Does This All Mean?
This study is pretty groundbreaking because it’s the first time anyone has really dug into *peritumoral* ultrasound radiomics specifically for predicting pCR to NAC, especially comparing it head-to-head with intratumoral radiomics and standard clinical factors using multiple ML methods.
The finding that PURS performs better than clinicopathologic factors is exciting. It suggests that the ‘neighborhood’ around the tumor, captured through these detailed radiomics features from a simple ultrasound, holds valuable information about how the cancer will respond to treatment. Even though IURS was the strongest predictor in this study, PURS still offers a significant boost over relying just on patient characteristics and tumor subtypes.
Why might the peritumoral region matter? As mentioned, it’s thought to be a ‘reactive zone’ full of immune cells and other elements that interact with the tumor and could influence how chemo works (or doesn’t work). The radiomics features extracted likely capture subtle textures and patterns in this area that we can’t easily see, reflecting this complex environment.
Speaking of features, the study found that certain types of features, particularly those derived from something called ‘wavelet transform’, were really important predictors in both PURS and IURS models. Wavelet transform basically breaks down the image into different frequencies, revealing textures and details that might be hidden in the original image. Features related to texture patterns (like GLCM, GLDM, GLRLM, GLSZM) were also key, reflecting the roughness or unevenness of the tissue.
And the ML algorithm star? Random Forest. Its ability to handle lots of complex data and avoid getting tripped up by noise seems to make it a great fit for analyzing radiomics features.

It’s also worth noting that while factors like tumor size or proliferation rate (Ki67) didn’t show a significant difference between responders and non-responders in this study, molecular subtypes (HER2+, Triple Negative, HR+/HER2-) were strongly associated with pCR, which aligns with what we already know. HER2+ tumors were most likely to respond completely, and HR+/HER2- were the least likely. This reinforces that tumor biology is crucial, but radiomics seems to add another predictive layer.
Looking Ahead (and a Few Caveats)
This study offers a really promising glimpse into the future of personalized cancer treatment. Using readily available ultrasound images and powerful machine learning, we might be able to get a much better idea of who will benefit most from NAC. This could lead to more informed decisions, potentially sparing some patients unnecessary toxicity or guiding others towards alternative or intensified treatments earlier.
Of course, like any research, this study has its limitations. It was a retrospective study done at a single center, meaning the findings need to be confirmed in larger, multi-center studies. They also had to exclude certain types of tumors or those where the peritumoral region wasn’t clearly visible on ultrasound, which could introduce some bias. And while they looked at clinicopathologic factors, they didn’t build separate models for each molecular subtype due to sample size, nor did they include genetic data, which is another piece of the puzzle.
Despite these points, the core message is strong: peritumoral ultrasound radiomics, especially when analyzed with sophisticated machine learning like Random Forest, is a novel and potentially powerful tool. It adds significant predictive value beyond standard clinical factors and could become a valuable part of the decision-making process for LABC patients considering NAC. It’s another step towards truly personalized cancer care, using the data we already have in smarter ways.
Source: Springer