Tiny Bubbles, Big Trouble: How Breast Cancer Exosomes Hurt Your Heart During Chemo
Alright, let’s talk about something super important, something that hits close to home for so many people. We’re diving into the fascinating, and frankly a bit scary, world where cancer treatment meets heart health. Specifically, we’re looking at how fighting breast cancer with a powerful drug called **Doxorubicin (DOX)** can sometimes cause serious damage to the heart. It’s a real balancing act, isn’t it? You need this potent weapon to fight the cancer, but it comes with a risk to another vital organ. For years, we’ve known DOX can be tough on the heart, leading to something called **cardiotoxicity**. But *how* exactly does this happen, especially when you consider the bigger picture – the cancer itself? That’s where things get really interesting.
The Problem: Doxorubicin’s Double Edge
So, **DOX** is a superstar in the world of chemotherapy. It’s incredibly effective against various cancers, including breast cancer, leukemia, and lymphoma. It’s saved countless lives. But, and it’s a big but, its use is often limited by its potential to cause severe, sometimes life-threatening, heart damage. We’re talking about things like weakened heart function, even heart failure. Imagine surviving cancer only to face a major heart problem later. That’s the challenge we’re trying to understand and overcome.
Beyond Direct Damage: The Crosstalk
Now, traditionally, we’ve focused on how **DOX** directly zaps heart muscle cells (cardiomyocytes). And yes, it does that through various nasty ways – messing with energy factories (mitochondria), damaging DNA, causing stress. But what if the cancer itself is also part of the problem? What if the tumor and the heart are actually *talking* to each other in a way that makes the heart damage worse? This idea of “cross-organ communication” is gaining traction in research. It’s like the tumor isn’t just sitting there; it’s actively sending signals that can influence distant organs, including the heart. We’ve seen hints of this before – for example, heart injury might even encourage cancer growth, and conversely, cancer can affect heart function. It’s a two-way street of pathological communication.
Exosomes: Tiny Messengers of Trouble
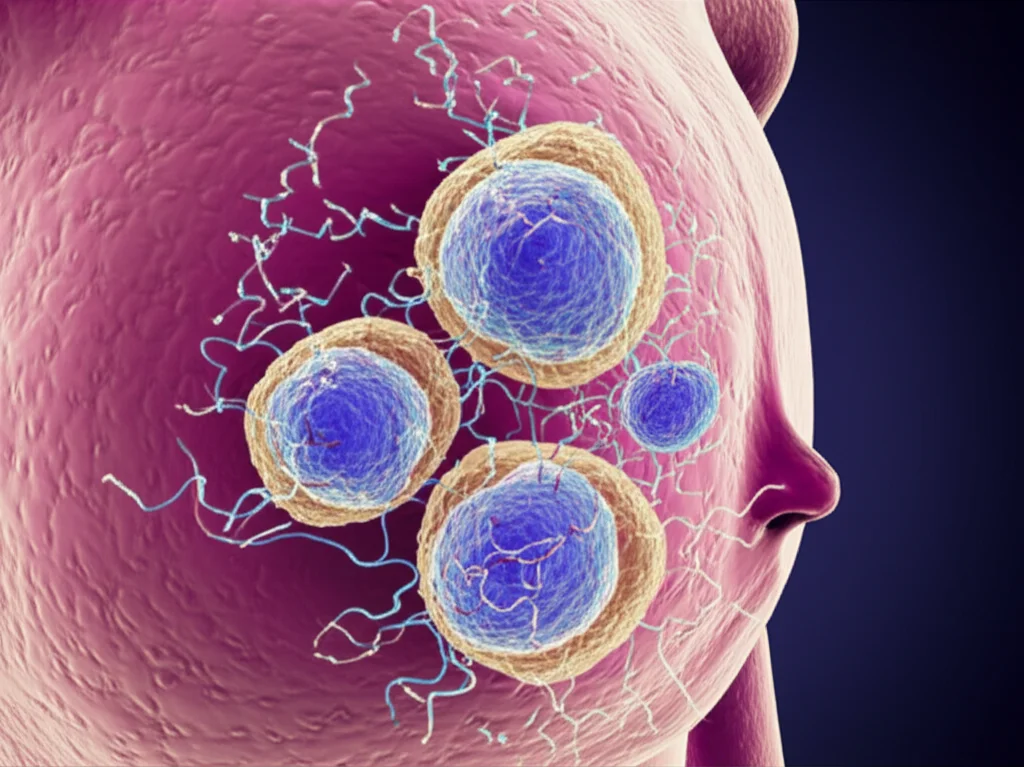
How do organs talk to each other over a distance? Well, one major way is through tiny little packages called **exosomes**. Think of them as microscopic bubbles, released by cells, that travel through the bloodstream carrying all sorts of cargo – proteins, genetic material like **microRNAs (miRNAs)**, and other molecules. They’re basically cellular mail carriers. Cells use them all the time for normal communication, but in disease, especially cancer, these exosomes can become carriers of harmful messages. Tumor cells are particularly good at pumping out exosomes. And it turns out, these tumor-derived exosomes can influence cells far away, preparing other tissues for cancer spread or messing with their function. This got us thinking: could exosomes from breast cancer cells be carrying a message that makes the heart more vulnerable to **DOX**?

We decided to investigate this idea. We grew heart muscle cells (both from mice and human stem cells) and breast cancer cells together in a dish, separated by a barrier that lets small things like exosomes pass through. When we added **DOX**, we saw that the heart cells co-cultured with breast cancer cells got *much* sicker than those treated with **DOX** alone. They showed classic signs of a specific type of cell death called **pyroptosis**, which looks like the cells are swelling up and forming bubble-like protrusions before they die. It was clear the breast cancer cells were sending *something* that aggravated the **DOX** damage.
We then isolated the exosomes specifically from breast cancer cells that had been treated with **DOX**. When we added these “DOX-induced breast cancer exosomes” (let’s call them D-BCC-EXOs) to heart cells, they were taken up, and *bam!* The heart cells showed increased signs of **pyroptosis** and damage, much more than when we added exosomes from untreated breast cancer cells. This was a big clue! It strongly suggested that something *within* these specific exosomes was the culprit. We even did experiments in mice with breast cancer, giving them D-BCC-EXOs, and saw that their hearts were more severely damaged by **DOX** compared to mice given normal breast cancer exosomes. Blocking exosome release from the tumors in mice also reduced the extra heart damage. This really solidified the idea that the tumor-heart communication via exosomes is a key player in this problem.
Unmasking the Culprit: miR-216a-5p
So, what exactly is this harmful message inside the D-BCC-EXOs? Since **miRNAs** are known to be important cargo in exosomes and can regulate gene expression, we decided to look closely at the **miRNAs** within these exosomes. We analyzed the **miRNAs** in exosomes from the blood of mice with breast cancer treated with **DOX**. We found several **miRNAs** that were significantly increased. Through a careful process of checking which of these were also high in breast cancer cell exosomes and which ones actually caused heart cell damage when introduced, we identified a prime suspect: **miR-216a-5p**.
It turns out, **miR-216a-5p** was significantly upregulated in exosomes from **DOX**-treated breast cancer cells and tissues, and importantly, its levels were also higher in the hearts of mice receiving these exosomes. When we experimentally increased **miR-216a-5p** in heart cells, they became much more susceptible to **DOX**-induced death and **pyroptosis**. Conversely, blocking **miR-216a-5p** in heart cells protected them. This was a smoking gun! **miR-216a-5p** carried by breast cancer exosomes seems to be a key driver of the extra heart damage. We even looked at blood samples from breast cancer patients treated with **DOX** who developed cardiotoxicity and found higher levels of **miR-216a-5p** in their plasma exosomes, correlating with worse heart function.
The Journey: From Tumor to Heart
Okay, so **miR-216a-5p** is the bad guy. But how does **DOX** cause breast cancer cells to load up their exosomes with it? We dug into the mechanisms within the breast cancer cells themselves. We found that **DOX** treatment increases the activity of a protein called **ATF3** (AMP-dependent transcription factor 3) in breast cancer cells. **ATF3** is a transcription factor, meaning it controls the expression of other genes. We discovered that **ATF3** directly binds to the region of DNA that controls the production of **miR-216a-5p**, essentially acting like a switch that turns up its production when **DOX** is around.
Once **miR-216a-5p** is made, it needs to get packaged into the exosomes. This process is often selective, controlled by specific RNA-binding proteins. We looked for proteins that might grab onto **miR-216a-5p** and guide it into exosomes. Our search pointed to a protein called **SF3B4**. We found that **SF3B4** specifically binds to **miR-216a-5p** and is crucial for packaging it into breast cancer exosomes. If we blocked **SF3B4** in breast cancer cells, less **miR-216a-5p** ended up in the exosomes, and these exosomes were less damaging to heart cells.
So, the chain of events in the breast cancer cell looks like this: **DOX** exposure -> increased **ATF3** -> increased production of **miR-216a-5p** -> **SF3B4** grabs **miR-216a-5p** -> **miR-216a-5p** gets packed into exosomes -> exosomes are released.
Inside the Heart: The Damage Mechanism
Now, let’s follow the exosome carrying **miR-216a-5p** to the heart cell. Once inside, the **miR-216a-5p** gets released and starts doing its work. **miRNAs** typically work by binding to specific target messenger RNAs (mRNAs) and causing them to be degraded or blocked, thus reducing the amount of the corresponding protein. We searched for potential targets of **miR-216a-5p** in heart cells that could explain the increased **pyroptosis**. Our analysis and experiments pointed to a protein called **ITCH** (Itchy E3 ubiquitin-protein ligase). We found that **miR-216a-5p** directly binds to the mRNA of **ITCH** and causes its levels to drop in heart cells.
Why is losing **ITCH** bad for the heart cell? **ITCH** is an enzyme that helps tag other proteins for degradation through a process called ubiquitination. One of the proteins that **ITCH** normally helps keep in check is called **TXNIP** (Thioredoxin-interacting protein). When **ITCH** levels drop because of **miR-216a-5p**, **TXNIP** is no longer properly ubiquitinated and degraded, so its levels go up.
And **TXNIP** is a known troublemaker! High levels of **TXNIP** are known to activate a complex protein machine in the cell called the **NLRP3 inflammasome**. When the **NLRP3 inflammasome** gets activated, it triggers a cascade that leads to the activation of other proteins, like Caspase-1 and GSDMD, ultimately resulting in **pyroptosis**, that bubbly, inflammatory cell death we saw.
So, the damage pathway in the heart cell looks like this: Exosomal **miR-216a-5p** uptake -> decreased **ITCH** -> increased **TXNIP** (due to less degradation) -> activation of **NLRP3 inflammasome** -> **pyroptosis** -> exacerbated **DOX** cardiotoxicity. It’s a complex but clear chain of events initiated by that tiny **miRNA** delivered by the exosome.
Hope on the Horizon: Potential Solutions
Understanding this detailed crosstalk mechanism opens up exciting new possibilities for protecting the hearts of breast cancer patients undergoing **DOX** chemotherapy. If the problem is harmful exosomes carrying a specific **miRNA**, maybe we can intervene at different points along this pathway.
* **Blocking Exosome Release:** We showed that blocking exosome release from the tumor using genetic methods (like knocking down Rab27a) reduced the extra heart damage in mice. While directly blocking exosome release in patients might be complex, this proves the concept.
* **Targeting the miRNA in the Heart:** We used a special tool called an **AAV9 miR-216a-5p sponge** delivered specifically to the heart muscle in mice. This “sponge” soaks up the **miR-216a-5p**, preventing it from doing its damage. This approach significantly protected the mice’s hearts from **DOX**-induced injury, even in a more clinically relevant mouse model using human breast cancer tissue. This suggests that targeting **miR-216a-5p** specifically in the heart could be a promising therapeutic strategy.
* **Targeting Downstream Players:** Since the damage pathway involves **TXNIP**, **NLRP3**, and Caspase-1, we also tested small molecules that inhibit these proteins. Inhibitors for Caspase-1 (VX765), **NLRP3** (MCC950), and **TXNIP** (SRI-37330) all showed protective effects on the heart in mouse models. This suggests that targeting these downstream components of the **pyroptosis** pathway could also be beneficial.

What This Means for Patients
This research provides crucial new insights into why **DOX** is so cardiotoxic, highlighting the previously underappreciated role of the breast cancer tumor itself in exacerbating the damage through exosomal communication. It means that managing **DOX** cardiotoxicity isn’t just about protecting the heart from the drug directly; it’s also about considering how the tumor is influencing the heart.
The findings suggest potential new strategies:
* Biomarkers: Measuring levels of **miR-216a-5p** in the blood exosomes of breast cancer patients before or during chemotherapy might help identify those at higher risk of developing cardiotoxicity, allowing for closer monitoring or preventative measures.
* Therapeutics: Developing therapies that specifically target **miR-216a-5p** in the heart, block the release of harmful exosomes from the tumor, or inhibit the downstream **pyroptosis** pathway could offer new ways to protect patients’ hearts without compromising the effectiveness of their cancer treatment.

Conclusion
In summary, we’ve uncovered a novel and critical pathway involving the transfer of **pro-pyroptotic miR-216a-5p** via exosomes from **DOX**-treated breast cancer cells to cardiomyocytes. This tiny **miRNA**, produced under the influence of **ATF3** and packaged by **SF3B4** in the tumor, travels to the heart, where it reduces **ITCH**, increases **TXNIP**, activates the **NLRP3 inflammasome**, and drives heart cell **pyroptosis**, making **DOX** cardiotoxicity worse. This complex **breast cancer-heart pathological crosstalk** is a significant factor. But the good news is, by understanding this mechanism, we’ve identified several potential targets – from blocking the exosomes themselves to specifically inhibiting **miR-216a-5p** in the heart or interfering with the downstream damage pathway. This research is a vital step towards developing better strategies to protect the hearts of cancer patients, allowing them to receive the life-saving treatments they need with fewer devastating side effects. It’s a challenging problem, but we’re getting closer to solving it, one tiny exosome at a time.
Source: Springer







