Unlocking Bacterial Survival: The Alarmone-GTP Switch Against Antibiotics
Hey there! Let’s chat about something super important, something that affects all of us, even if we don’t see it happening: bacteria and antibiotics. You know how sometimes you take antibiotics to get rid of a nasty infection, but some sneaky bacteria just seem to hang around, making things tricky? Well, those tough little survivors are often called ‘persisters’. They’re not genetically resistant – they haven’t mutated to shrug off the drug forever – they’ve just entered a kind of dormant state, a temporary hideout where the antibiotic can’t touch them. Scientists have been scratching their heads for ages trying to figure out *how* they do this. It’s like they have a secret switch they flip to go into survival mode.
And guess what? A fantastic piece of research, the one we’re diving into today, seems to have found a key part of that secret! It points to a shared molecular pathway, a kind of internal signal system, that bacteria use to become these antibiotic-defying persisters. It involves two cool molecules: an ‘alarmone’ called (p)ppGpp and a fundamental energy/building block molecule called GTP. Think of it like a tiny, internal switch that controls whether the bacterium is actively growing and vulnerable, or chilling out in a protected, dormant state.
What Are Persisters, Anyway?
So, as I mentioned, persisters are individual bacterial cells that can survive antibiotic treatment even though their genetic makeup says they should be killed. Joseph Bigger first spotted this phenomenon way back in the 1940s! Since then, we’ve learned they can pop up in a few ways:
- Starvation-triggered: When times get tough, like when nutrients run low.
- Spontaneous: Just appearing randomly in a growing population, even when things are good.
- Antibiotic-induced: Sometimes, the antibiotic itself can trigger their formation.
For the longest time, the exact molecular recipe for making a persister cell was a bit fuzzy. People thought maybe it was just slow growth, or low energy levels (ATP). But this new study, focusing on the bacterium Bacillus subtilis (a common soil bug, but a great model for many others), really narrows it down.
The Alarmone Connection: (p)ppGpp Steps In
Okay, let’s talk about the first molecule in our dynamic duo: (p)ppGpp. This is known as a bacterial ‘alarmone’. It’s like the cell’s stress signal. When things go wrong – like amino acid starvation or energy depletion – (p)ppGpp levels shoot up. Previous work hinted that this alarmone was involved in antibiotic survival, but its exact role in *persistence* (that deep dormancy, not just slow growth tolerance) wasn’t totally clear.
This research used mutant strains of B. subtilis that couldn’t make (p)ppGpp. And bam! They saw a massive reduction in persister formation across the board. Not just a little less, but a *tenfold* drop! This tells us that (p)ppGpp isn’t just *correlated* with persistence; it’s pretty much *necessary* for it. What’s more, they found that *forcing* the bacteria to make (p)ppGpp, even when they weren’t stressed, was enough to create a bunch of persisters. So, (p)ppGpp accumulation is both necessary *and* sufficient to trigger this state. Pretty powerful stuff for a little molecule!

Enter GTP: The Real Switch Operator
Now, here’s where it gets really interesting. If (p)ppGpp is the alarm, what’s the action it triggers? The study points to GTP (guanosine triphosphate). GTP is a vital molecule for bacteria – it’s used for making DNA, RNA, proteins, and lots of other essential cell parts. (p)ppGpp is known to be a bit of a bully to GTP; it inhibits the enzymes that make GTP and even competes with GTP for binding to important cellular machinery.
The researchers found that when (p)ppGpp levels rise, GTP levels plummet. And here’s the kicker: they managed to create a mutant strain where they could lower GTP levels *without* inducing (p)ppGpp. And guess what? Lowering GTP *alone* was enough to significantly increase persister formation! This strongly suggests that GTP depletion is the critical downstream event, the actual trigger that puts the brakes on the cell and sends it into dormancy, leading to persistence.
This is a big deal because it clarifies the mechanism. It’s not just stress (signaled by (p)ppGpp); it’s the *consequence* of that stress on a specific molecule, GTP, that matters for persistence.
Seeing is Believing: Single-Cell Insights
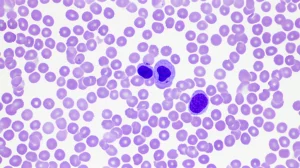
One of the coolest parts of this research is how they actually *saw* this happening in individual cells. Persisters are rare outliers in a population, so looking at the average behavior of millions of cells doesn’t tell you much about how a single cell decides to become a persister. They developed a clever fluorescent reporter system (they called it PlowGTP) that glows brightly when GTP levels in a single cell drop low.
Using this reporter and fancy microscopy, they could watch cells in real-time. They saw that most cells had high GTP (low fluorescence) and grew happily. But a small, rare subpopulation of cells showed high fluorescence, meaning low GTP. And these low-GTP cells? They were the ones that survived antibiotic treatment! They even used cell sorting (like sorting MeMs, but with bacteria) to isolate the low-GTP cells, and confirmed that nearly all of them were persisters.

What was truly fascinating was watching the transition. They saw actively growing cells where the GTP reporter fluorescence would gradually increase over time, even across cell divisions. Then, suddenly, when the fluorescence (and thus, low GTP) hit a specific threshold, the cell would just *stop* growing. Boom. Switched into dormancy. This wasn’t a slow fade; it was a rapid, switch-like event triggered by hitting that critical low-GTP level. This single-cell view is crucial because it shows persistence isn’t just slow growth across the board; it’s a distinct phenotypic switch in individual cells.
Different Paths, Same Destination
The study also looked at how the different ways persisters form (starvation, spontaneous, antibiotic-induced) connect to this (p)ppGpp-GTP switch. Turns out, they all converge on this pathway, but they use different ‘alarmone synthetases’ – the enzymes that actually make (p)ppGpp – to get there.
- Starvation-triggered persistence: This mainly relies on one specific synthetase called Rel.
- Spontaneous persistence: This is a bit more complex, involving both Rel and another synthetase called SasB. Interestingly, SasB seems to have a self-amplifying mechanism, which might explain how these persisters can pop up randomly even without a strong external stress signal.
- Antibiotic-induced persistence: This was particularly cool. They found that cell-wall-targeting antibiotics (like vancomycin or bacitracin) induce persistence by activating a *third* synthetase, SasA. This means the antibiotic itself triggers the (p)ppGpp accumulation via SasA, leading to GTP depletion and persistence. It’s like the bacteria sense the damage and preemptively go into hiding!
So, regardless of the initial trigger, the pathway seems to lead to increased (p)ppGpp, decreased GTP, and the flip of that survival switch. It’s a shared strategy for dealing with different kinds of threats.

Why This Matters for Us
Okay, so why should we care about bacterial alarmones and GTP levels? Because these persisters are a major headache in treating infections. They survive the initial antibiotic onslaught, and when the drug is gone, they wake up and can re-establish the infection. This often leads to chronic or recurring infections that are super difficult to clear. Plus, surviving antibiotic treatment gives bacteria more chances to *develop* true genetic resistance, which is a growing global crisis.
This research gives us a brand new target. Instead of just focusing on killing actively growing bacteria, maybe we can develop drugs that prevent bacteria from flipping that persistence switch in the first place. If we can stop them from depleting GTP or block the (p)ppGpp signal, we might be able to keep them vulnerable to antibiotics.
It also helps explain why some antibiotic treatments are more effective than others, or why combination therapies might work better. Understanding which synthetase (Rel, SasB, SasA) is involved in different scenarios could help tailor treatments.
Wrapping It Up
So there you have it. This study provides compelling evidence that Bacillus subtilis, and likely many other bacteria (especially those in the same family, like the dreaded Staphylococcus aureus), use a common, underlying mechanism to become persisters: the alarmone (p)ppGpp accumulates, leading to a critical drop in GTP levels, which flips a rapid, switch-like entry into a dormant, antibiotic-tolerant state. It’s a clever survival strategy, but now that we’re starting to understand its molecular nuts and bolts, maybe, just maybe, we can find ways to disarm it.
This kind of fundamental research is so exciting because it peels back the layers on how these microscopic organisms survive and adapt. It gives us hope that we can stay one step ahead in the ongoing battle against infectious diseases.
Source: Springer